Plain-film imaging of the sacrum and coccyx are often difficult because of obstructing factors such as the bowel, bladder, clothing artifact, and patients who are difficult to penetrate due to obesity.
Clothing artifact management and tight collimation are easily achieved. Putting a patient in a gown for pelvic X-ray eliminates clothing artifacts. One never knows what the patient will have in or on their jeans / other garments. Even the thread in the material can be an obstruction. If the AP sacrum and coccyx views are performed PA, there is a significant reduction in radiation exposure with no loss in diagnostic image.
Shielding for males is recommended; however, for females it is not possible. Therefore, it is very important to screen women of childbearing age for possible pregnancy prior to imaging the pelvis. Close collimation improves detail when the part is small and reduces scatter.
 Figure 1: Landmarks for PA sacrum and coccyx.
Routine views of the sacrum are an AP (PA) sacrum, AP (PA) coccyx and lateral sacrum/coccyx. When the sacroiliac joints are the specific area of interest, right and left posterior oblique views can be included.
Figure 1: Landmarks for PA sacrum and coccyx.
Routine views of the sacrum are an AP (PA) sacrum, AP (PA) coccyx and lateral sacrum/coccyx. When the sacroiliac joints are the specific area of interest, right and left posterior oblique views can be included.
It is important that the pelvis is properly positioned so the sacrum and sacroiliac joints are symmetrically displayed. When accurately positioned, the PA sacrum view will demonstrate the median sacral crest aligned with the symphysis pubis and the ischial spines equally demonstrated in relationship to the pelvic brim. The patient stands facing the bucky as close as possible. Check feet and torso for rotation. Measure thickness at the level of the trochanters. Tube angle is 15° caudal to reduce foreshortening of the sacrum. Locate the PSIS and place the horizontal CR (central ray) 1-2 inches below the PSIS or mid-sacrum. The vertical CR is the mid-sagittal plane. (Figure 1)
 Figure 2: PA view of the sacrum.
Collimation is slightly less than the film size (8 x 10 portrait). A properly positioned PA sacrum view will demonstrate the entire fifth lumbar vertebra, symphysis pubis, and both sacroiliac joints. (Figure 2)
Figure 2: PA view of the sacrum.
Collimation is slightly less than the film size (8 x 10 portrait). A properly positioned PA sacrum view will demonstrate the entire fifth lumbar vertebra, symphysis pubis, and both sacroiliac joints. (Figure 2)
When imaging the coccyx, proper positioning and optimal exposure technique are essential to producing a diagnostic radiograph. Because the coccyx is positioned forward (kyphotic curvature) relative to the sacrum, it is not visualized anatomically with the AP sacrum. Often the pelvic brim will obstruct the coccyx unless the patient and central ray are properly aligned. When properly positioned, the PA coccyx radiograph will demonstrate the coccyx aligned with the symphysis pubis and at equal distance from the lateral wall of the pelvic inlet. (Figure 3)
 Figure 3: PA view of the coccyx.
To obtain a PA coccyx, the patient stands facing the bucky as close as possible. Check feet and torso for rotation. Measure thickness at the level of the trochanters. Tube angle is 10° cephalad. Place the horizontal CR 1-2 inches above the trochanters. The vertical CR is the mid-sagittal plane. (Figure 1) Collimation is slightly less than the film size (8 x 10 portrait).
Figure 3: PA view of the coccyx.
To obtain a PA coccyx, the patient stands facing the bucky as close as possible. Check feet and torso for rotation. Measure thickness at the level of the trochanters. Tube angle is 10° cephalad. Place the horizontal CR 1-2 inches above the trochanters. The vertical CR is the mid-sagittal plane. (Figure 1) Collimation is slightly less than the film size (8 x 10 portrait).
The exposure for adults is generally between 75 and 85 kVp; however, to achieve good recorded detail, one should also employ the following techniques: 1) instruct the patient to remain still during exposure; 2) suspend ventilation during exposure; 3) use the shortest OID; and 4) use the smallest focal spot size available. The bladder and colon should be emptied prior to imaging the sacrum or the coccyx.
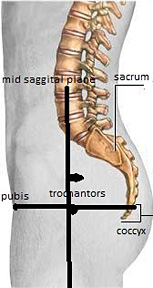 Figure 4: Landmarks for lateral sacrum / coccyx. Vertical CR is 2" posterior to mid-coronal plane (note arrow).
The lateral view of the sacrum/coccyx is performed with the patient in the standing / lateral position and the central ray directed vertical (perpendicular) to the sacrum. The purpose of the lateral view is to demonstrate the fifth lumbar vertebra, entire sacrum, and coccyx free of superimposition by fecal material and gas, and without the urinary bladder and rectum obstructing viewing. Notwithstanding, proper positioning of the sacrum / coccyx in a true lateral is an essential diagnostic criterion. Patient stands in lateral position with feet shoulder-width apart. Have patient cross arms at shoulder level. Locate the iliac crest and symphysis pubis. The horizontal CR is midway between iliac crest and symphysis pubis. The vertical CR is 2-3 inches posterior to the mid-coronal plane. Center film to horizontal CR. Collimation is slightly less than film size. (Figure 4)
Figure 4: Landmarks for lateral sacrum / coccyx. Vertical CR is 2" posterior to mid-coronal plane (note arrow).
The lateral view of the sacrum/coccyx is performed with the patient in the standing / lateral position and the central ray directed vertical (perpendicular) to the sacrum. The purpose of the lateral view is to demonstrate the fifth lumbar vertebra, entire sacrum, and coccyx free of superimposition by fecal material and gas, and without the urinary bladder and rectum obstructing viewing. Notwithstanding, proper positioning of the sacrum / coccyx in a true lateral is an essential diagnostic criterion. Patient stands in lateral position with feet shoulder-width apart. Have patient cross arms at shoulder level. Locate the iliac crest and symphysis pubis. The horizontal CR is midway between iliac crest and symphysis pubis. The vertical CR is 2-3 inches posterior to the mid-coronal plane. Center film to horizontal CR. Collimation is slightly less than film size. (Figure 4)
 Figure 5: Lateral view of the sacrum and coccyx.
When properly aligned, the apophyseal joints of L5/S1 are superimposed, the greater sciatic notches are superimposed, the sacral canal is opened and the median sacral crest is in profile. On the lateral sacrum / coccyx, structures demonstrated include the entire fifth lumbar vertebra, entire sacrum / coccyx, and proper visualization of an opened sacral canal. The coccyx should not be overexposed, showing good recorded detail. (Figure 5) It may be necessary to use a high grid ratio and contact lead along the collimated edge of the field to reduce scatter radiation reaching the image receptor.
Figure 5: Lateral view of the sacrum and coccyx.
When properly aligned, the apophyseal joints of L5/S1 are superimposed, the greater sciatic notches are superimposed, the sacral canal is opened and the median sacral crest is in profile. On the lateral sacrum / coccyx, structures demonstrated include the entire fifth lumbar vertebra, entire sacrum / coccyx, and proper visualization of an opened sacral canal. The coccyx should not be overexposed, showing good recorded detail. (Figure 5) It may be necessary to use a high grid ratio and contact lead along the collimated edge of the field to reduce scatter radiation reaching the image receptor.
Click here for more information about Deborah Pate, DC, DACBR.





