In my first article on discogenic pain, I talked about using midline tenderness as a diagnostic tool indicating inflammation of the disc. I use the digital interspinous pressure (DIP) test to assess the state of the deep midline structures.
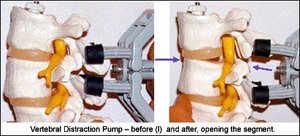
What are my chiropractic adjustive techniques for midline tenderness and discogenic pain? I use a variety of low-force techniques, but for this article, I'll share my basic tools for eliminating what I call a "true positive" for midline tenderness. This means that after I've corrected the rest of the pelvis and lumbar subluxations, the midline tenderness remains. My favorite tool to correct this is the vertebral distraction pump (VDP), used via the following protocol. This simple device allows us to effectively distract two vertebrae from each other. The images below illustrate its "in vitro" effects. Flexion-distraction tables are also effective for Y-axis or axial distraction, especially for the lower lumbar vertebrae.
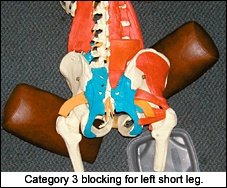
 I have a strong preference for using the VDP to correct vertical compression. Here's the protocol I follow: I find the tender spots and mark them with a pen. I decide which one is primary by inhibition testing, or by assessing which one is more tender. I then assess for short leg and block the patient utilizing sacral-occipital technique, category 3. This means that on the short-leg side, the block is low, under the trochanter, and points obliquely downward. The upper block is under the iliac crest on the long-leg side, and also points obliquely downward. The blocks do not point toward each other; both are pointing about 45 degrees downward. If this is the correct blocking position, when I go back to the inflamed tender level, the tenderness will usually be somewhat diminished. If not, I play with the angle on the lower block, or even try reversing the blocking. On rare cases, it works better to just bilaterally block under the ilium, with the blocks directly across from each other. Again, diminishment of tenderness is my guide here.
I have a strong preference for using the VDP to correct vertical compression. Here's the protocol I follow: I find the tender spots and mark them with a pen. I decide which one is primary by inhibition testing, or by assessing which one is more tender. I then assess for short leg and block the patient utilizing sacral-occipital technique, category 3. This means that on the short-leg side, the block is low, under the trochanter, and points obliquely downward. The upper block is under the iliac crest on the long-leg side, and also points obliquely downward. The blocks do not point toward each other; both are pointing about 45 degrees downward. If this is the correct blocking position, when I go back to the inflamed tender level, the tenderness will usually be somewhat diminished. If not, I play with the angle on the lower block, or even try reversing the blocking. On rare cases, it works better to just bilaterally block under the ilium, with the blocks directly across from each other. Again, diminishment of tenderness is my guide here.
 Next, using the VDP, I distract the vertebrae from each other for 4-6 repetitions, holding for 10 seconds each time. I call my VDP my "hands of Shaquille O'Neal," because it gives me stronger hands. The VDP is better for giving more leverage, and by applying the pressure paraspinally, it's not painful to the patient. The VDP is placed so it straddles the interspinous space, without touching any tender spots.
Next, using the VDP, I distract the vertebrae from each other for 4-6 repetitions, holding for 10 seconds each time. I call my VDP my "hands of Shaquille O'Neal," because it gives me stronger hands. The VDP is better for giving more leverage, and by applying the pressure paraspinally, it's not painful to the patient. The VDP is placed so it straddles the interspinous space, without touching any tender spots.
If you don't have a VDP or a distraction table, the procedure can be done manually. Place one hand on the sacrum and place the pisiform, or first metacarpophalangeal joint, against the lower border of the spinous, just above the tender involved level. Separate for 7-10 seconds, then release. Repeat 4-6 times.
With my second hand on the sacrum. I take the sacrum inferior and anterior as I distract the interspinous space. This adds a component of dural distraction. I follow the craniosacral rhythm as I do this, distracting in the expansion phase as the sacrum moves anterior. I relax my distraction in the relaxation phase of the cranial rhythm. If you don't know how to follow the cranial rhythm, just distract for 10 seconds, then relax for a few seconds.
 Regardless of the method you use, when you are done, the interspinous space should be much less tender. If you had two tender levels, check the one you didn't correct. If it is no longer tender, you are done. If it is still tender, perform the same procedure on that level. In an inflamed disc, you will probably need to conduct the procedure several times over a few weeks, as discs are tough to change rapidly.
Regardless of the method you use, when you are done, the interspinous space should be much less tender. If you had two tender levels, check the one you didn't correct. If it is no longer tender, you are done. If it is still tender, perform the same procedure on that level. In an inflamed disc, you will probably need to conduct the procedure several times over a few weeks, as discs are tough to change rapidly.
If the tenderness is only minimally changed after this procedure, check the sides of the spinous processes at the involved level. If one side is extremely tender and resists lateral-to-medial motion, you may have a translation; a lateral subluxation (nonphysiological). Use the three methods - engage, listen and follow (ELF) - to gently push it lateral to medial. Recheck for tenderness, both on the side of the spinous and in the midline. Sometimes, this is the key. You can also place the VDP so that it is operating unilaterally, using only two legs of it angled obliquely on the tender side, and distract there.
I remind you to not chase after symptoms or painful spots. You need to check the whole spine; evaluate the pelvis, and check the lower extremity. Anything in the neurospinal axis can irritate the lumbar discs.
I am convinced that specific axial distraction is a key part of the chiropractic toolbox, and allows us to correct the spine and alleviate disc pain more effectively and quickly. Specific axial distraction, or variations of it, has been done thousands of times by James Cox, who popularized the use of flexion-distraction; by Bruce Broughton, who invented the VDP; and by many other DCs. It can be very effective for either a classic disc herniation, or for the occult internally disrupted disc.
My next article will introduce another technique for discs using the VDP (to which I have, incidentally, been recently introduced). It's already amazing me, but I need to use the technique on at least another 100 patients before I feel comfortable sharing it with you.
Resources
- Bruce Broughton, DC. Chiropractic Association of Oregon convention, 2001.
- Broughton, Bruce, Treatment of disc herniations with the distraction pump, Chiropractic Technique, May 1999; 11(2).
- Herb Freeman, DC, Keizer, OR: personal conversations.
- Cox, James. Articles, books and seminars on the use of flexion-distraction.
- Trauma, An Osteopathic Approach. Barral and Crobier. Eastland Press, 2001
- Heller, Marc. Discogenic pain, diagnosis and treatment. www.chiroweb.com/archives/21/18/08.html.
Click here for more information about Marc Heller, DC.





