The various movements of gait (lateral shifting, undulating, flexion/extension, figure eights and the myriads of personalized idiosyncratic motions) are included in the movement repertoire of the SIJ.
The gluteus medeus (g.med.) functions to protect the SIJ as well. During initiation of the stance phase of gait the g.med. on the closed chain side begins to keep the pelvis on the swing phase side from dropping abruptly. In this movement the speed of contraction of the g.med. is critical. If the g.med contraction is too late, the pelvis drops, as in a Trendelberg sign. Consequently, stabilization of the SIJ may be troublesome if the speed of activation of the g.med. is impaired or the muscle is truly weak.
Orthopedic testing of the SIJ and classic strength testing of the g.med. are often inadequate to detect this common gait dysfunction.
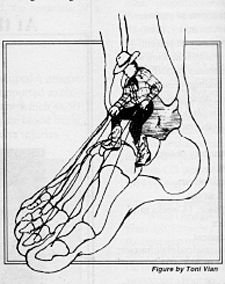
Any foot dysfunction, e.g., hyperpronation, may initiate a chain reaction which could possibly result in a SIJ disorder. Manipulation of the SIJ may frequently resolve symptoms in such cases. In cases which don't readily respond a broader rehabilitation approach may be required. Correction of the foot problem with manipulation, exercise, or orthoses may be necessary. Training of the g.med. to speed up its activation speed will also increase pelvic stability. If the foot dysfunction or the g.med. incoordination is not corrected, shearing stress across the SIJ may accumulate. Eventually, without any history of trauma the cumulative effects of microtrauma may lead to recurrences of SI pain.
Evaluation of the g.med may be performed in several ways: 1) observation of gait, as mentioned above; 2) in the side lying hip abduction coordination test, the upper leg is actively abducted and critical observation is made for any deviation made in hip flexion (tensor fascia lata), external hip rotation (piriformis), premature cephalad shifting (quadratus lumborum) of the pelvis, or backward rotation of the pelvis; 3) in the single leg standing test, the pelvis should remain level at the initiation of the single leg stance. There should be a discernible shift of more than one inch to the weightbearing side within the first 20 seconds of standing in the single leg stance. In brief this is how one may develop a rational suspicion that the relationship between the g. med. and the SIJ is impaired.
Ideally then a treatment that utilizes manipulation (as indicated) to free the SIJ recognizes the intimate relationship between muscle and joint, makes a dynamic assessment, trains the g.med. and SIJ as included in the locomotor system, and makes the exercise accessible yet challenging for the patient, will provide a more comprehensive approach to the evaluation and treatment of the SIJ syndrome.
Effective treatment of the entire motor system at some point must involve treating the system as a whole. Sensorimotor exercise recognizes the integration of the afferent and efferent aspects of the locomotor system and allows the practitioner to realize how all the elements come together and are expressed through gait and posture. Exercises that automatize postural and control of movement on a reflex, semi-automatic basis are part of sensorimotor training.
It is understood that treatment of the peripheral structures, i.e., joints, skin, muscles, allows ease of movement in areas treated, but may not automatically effect a centrally integrated and correct movement pattern. If it is our intention to improve function then we are obligated to assess function locally and globally, biomechanically and kinesiologically. The effectiveness of local treatment is assessed in light of global outcomes, i.e., posture and gait.
The goal of sensorimotor exercise is to integrate peripheral function with central programming. Movements that require conscious and willful activation may be monotonous and prematurely fatiguing to the participant. Whereas movements that are subcortical and reflexive in nature require less concentration, are faster acting and may be eventually automatized.
Proprioception loosely defined means the ability to receive and process sensory input. Sensory information enters the CNS from exteroceptors of the skin, position and movement detectors of the joints and muscles and is further correlated with information from visual and vestibular centers. This sensory information is formatted and reformatted in subcortical centers and then begins its efferent decent to the periphery where the actual movement is realized.
The Czech neurologist Janda's1 approach to sensorimotor begins from the ground up, with careful attention to formation of a shortened longitudinal arch without flexion of the toes. This is called the "short foot" and is based on the work of Freeman.2
It was Freeman who demonstrated that such a "short foot" position would increase proprioceptive outflow measurably. Exercises proceed from sitting to standing and from stabile to labile surfaces. The "short foot" position is maintained throughout most of the exercises.
Corrections in alignment are made from the ground up as well. This is consistent with the concept of the closed chain\kinetic chain reaction. In standing, various leaning movements are introduced and explored. Semi-squat positions that change the center of gravity slightly and require more work of the quads and gluts are also utilized. A single step taken forward with a forward lean and held there emphasizes alignment, coordination, and balance. The same is done with a single backwards step with the torso aligned upright and the ishia over the heels. These are fundamental movements that posture, gait and activities of daily living are built upon.
To elicit fast, reflexive responses the patient is "pushed" quickly but gently about the torso and shoulders. This challenges the patient to remain upright and respond to sudden changes in their center of gravity. These pushes are performed in two leg and in single leg standing with the eyes open. (Closing the eyes while performing these exercises focuses the participant's awareness on kinesthetic sense and is more challenging to perform).
This creates quick loss and re-establishment of balance with each push. Sudden changes in the center of gravity requires fast reflex responses to maintain balance and to protect joints from the untoward effects of uncoordinated and delayed muscle contraction.
To further challenge reflexive righting movements the subject is placed on a labile surface, i.e., the rocker board. The rocker board is unstable in one plane only. The patient may stand on the board facing in various directions to control the plane of instability. Again, the exercises proceed from two leg standing to single leg standing and pushes are utilized to elicit a fast response. Arm movements overhead, catching a ball, head turning, etc., are clever and fun ways to vary the center of gravity and made the program interesting.3
Mixing stabile and labile surfaces are more advanced skills. Hopping from floor to board, on two legs, on a single leg, mixing surfaces from rocker to wobble, etc., are ways to vary the terrain. One is limited only by one's imagination and the needs of the patient.
Janda has devised a unique pair of balance sandals consisting of a rigid sole configured to support the longitudinal arch and met heads as in the short foot. On the bottom of the sole a rigid hemisphere about the size of a tennis ball is fixed at the midway point. This essentially creates a pair of mini wobble boards to carefully walk upon. The effects are remarkable. In Janda's study1 after two weeks of prescribed exercise the speed of contraction of the g.max. and the g.med were increased by as much as 180 percent to 200 percent, and remained so as long as six weeks post-exercise without further reinforcement.
For patients who present with SIJ syndrome and have plateaued prior to a satisfactory outcome, this approach offers a means that has demonstrated measurable success in a rational manner. Pelvic instability often results from adaptation to injury, pathology or dysfunction in the lower extremity kinetic chain. Foot disorders and g.med. incoordination are the most important functional pathologies responsible for SIJ disorders. Rehabilitation of the entire kinetic chain is essential to treat chronic or recurrent SIJ problems.
References
- Bullock-Saxton, Janda, Bullock. Reflex activation of gluteal muscles in walking, Spine 18(6) pp 704-708, 1993.
- Freeman, Dean, Hanham. The etiology and prevention of functional instability of the foot. Journal of Bone and Joint Surgery 47B:687-685, 1965.
- Janda, Vavrova. Sensory Motor Stimulation.
Jerry Hyman, DC
Craig Liebenson, DC
Click here for previous articles by Craig Liebenson, DC.





