- Introductory Training - Graded Exposures to Grooved Stability Patterns
The introductory level of self-care advice includes biomechanical advice about how to avoid low back irritation during ADLs. Behavioral medicine or sports psychology tenets of "paced activity" and the relationship between hurt and harm should be discussed.2,6,7 Many LBP patients have excessive fear-avoidance beliefs or catastrophizing behaviors that promote a passive, symptom-driven approach, excessive pathoanatomic diagnositic testing, and a poor prognosis.12 At the other end of the spectrum are individuals who are overly aggressive, which can lead to a "boom or bust" mentality.
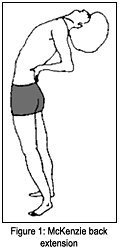
The middle path is best exhibited by the modern emphasis on quota-based "graded exposures" to feared stimuli.12 This operant conditioning model progressively demonstrates to patients that hurt does not necessarily equal harm, and that activity - contrary to the patients' beliefs - is actually beneficial.4 The activities chosen should be mutually agreed upon and should either reduce mechanical sensitivity (MS) or centralize symptoms, while being carried out to quota (a prescribed dosage). An example is a McKenzie exercise of spinal extension in a sciatica patient, which centralizes leg symptoms to the low back (figure 1).
Exercises should improve the patient's abnormal motor control (AMC). Most patients have poor kinaesthetic awareness of how to produce and/or control motion of their problem area. The patient learns to "discover" how to move and "cen-trate" an important region such as the lumbopelvic, scapulothoracic, or cervicocranial. The hip hinge and cat-camel are examples of exercises that teach this motor control (figures 2 and 3).
Trunk muscle coactivation by an abdominal bracing technique has been shown to increase the margin of stability when performing activities.6,18 Abdominal bracing involves coactivation of muscles in 360 degrees around the lumbar spine. Abdominal hollowing, which has been popularized by Australian researchers, is a very similar method. Bracing requires a light contraction of about 5 percent to 10 percent of a patient's maximum voluntary contraction ability. This is similar to being tickled or bearing down slightly.18-19 However, the key is that the breath is not held during the brace, and abdominal contraction is not entrained to a certain phase of respiration.
- Isolation of Specific Stability Patterns
Once a patient's functional range (range of motion without MS or AMC) begins to expand, it is necessary to further "groove" functional patterns by increasing the intensity of training, so as to achieve gains in endurance. McGill and colleagues have demonstrated that both muscle output and spinal load can be measured for a variety of exercises.1,15-16 Muscle output is determined as a percentage of maximum voluntary contraction ability (MVC) and spinal load as a measure of spinal compression and shear forces. Ideal exercises are those that have a high ratio of muscle challenge to spinal load.
Exercise science principles guide the selection of exercise intensity, frequency and duration. Motor control or stability training requires an emphasis on endurance, rather than strength.17,20,22 For this reason, the intensity of training is submaximal. As an example, a typical prescription would involve eight to 10 repetitions of slow movements with prolonged hold times (five to six seconds/repetitions, or about two breaths). A frequency of twice a day with a duration of up to three months is often required to remediate chronic spinal pain.14
McGill has developed the concept of "the big 3" in isolating and training stability patterns for the low back region.18 Such training encompasses low-load exercises with wide margins of safety/stability for the anterior, lateral and posterior musculature. Generally, loads under 3000N of force are considered safe for acute/subacute exercise training. Routine ADLs involve about 2000N and the NIOSH limit for repetitive tasks is 3300N.11 Table 1 shows the load profiles for a variety of low back exercises. Exercises with wide margins of stability should be performed after limbering up - and not immediately upon arising or after prolonged sitting.5,23,24 Good form or coordination is a prerequisite for such training.21
| Table 1 - Lumbar Spine Load Profiles for Common Exercises and Activities1,17-18 Safe in Acute LBP
Unsafe in Acute LBP
|
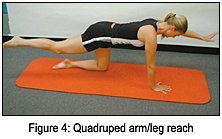
The quadruped position is used to train the back muscles. Once the quadruped single leg reach is mastered, movement in the opposite arm can be added (figure 4).
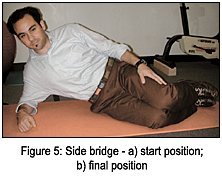
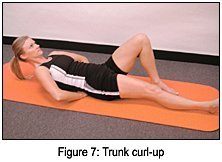
The lateral musculature is trained with the side bridge (figure 5). The abdominals can be trained with the supported dead bug (isometrically) (figure 6) and then progressed to a partial curl-up with spinal neutral control (slight lordosis) (figure 7).
- Integration - Functional Integrated Training (FIT)
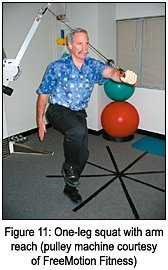
Unless functional training occurs, there is no guarantee that the individual will be stable during "real world" challenges. Examples of functional training include squats, lunges, pushing, pulling, catching, carrying, etc. (figures 10 and 11). Individuals engaged in demanding sports or occupations may require the addition of unstable surfaces such as balance boards and gymnastic balls to intensify the stability challenge.
Conclusion
Stability training is appropriate for sedentary, deconditioned individuals as well as fit athletes. In the acute phase, the margin of error is great, so exercises with wide margins of stability should be prescribed. As they recover or face increased motor system challenges in their daily lives, patients need exercises which can stabilize them in riskier situations. Since these exercises have lower margins of stabiity, the clinician must determine patients' readiness and need for them.
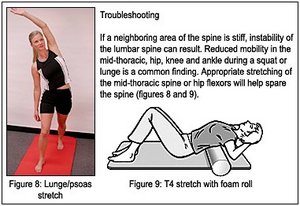
At each stage of spine stability, training appropriate movement patterns that stabilize the spine should be "grooved." Endurance and motor control are more important than strength and power in low back injury prevention. Flexibility/mobility are important, but primarily for surrounding areas above and below the lumbar spine.
It is not hard for chiropractors to integrate rehabilitation into their practices. A step-wise approach has been developed which is both effective and efficient.
References
- Axler CT, McGill SM. Low back loads over a variety of abdominal exercises: searching for the safest abdominal challenge. Med Sci Sports Exerc 1987; 29:804-810.
- Butler D, Moseley L. Explain Pain. Noigroup Publications, Adelaide, Australia, 2003.
- Cholewicki J, McGill SM. Mechanical stability of the in vivo lumbar spine: implications for injury and chronic low back pain. Clin Biomech 1996;11(1):1-15.
- Crombez G, Vlaeyen JW, Heuts PH, et al. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain 1999;80:329-39.
- Green J, Grenier S, McGill SM. Low back stiffness is altered with warmup and bench rest: Implications for athletes. Med Sci Sports Exerc 2002; 34(7):1076-1081.
- Harding VR, Simmonds MJ, Watson PJ. Physical therapy for chronic pain. Pain - Clinical Updates, International Association for the Study of Pain 1998;6:1-4.
- Harding V, Williams AC de C. Extending physiotherapy skills using a psychological approach: Cognitive-behavioural management of chronic pain. Physiotherapy 1995;81:681-687.
- Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine 2001;26:e243-e248.
- Indahl A, Haldorsen EH, Holm S, et al. Five-year follow-up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine 1998;23:2625-2630.
- Kool J, de Bie R, Oesch P, Knusel O, et al. Exercise reduces sick leave in patients with non-acute non-specific low back pain: a meta-analysis. J Rehabil Med 2004;36:49-62.
- Liebenson C. What's all the buzz about spinal stability? Part one: biomechanics and neurophysiology. Dynamic Chiropractic, June 3, 2004;22 (12). www.chiroweb.com/archives/22/12/13.html.
- Linton SL (ed). New avenues for the prevention of chronic musculoskeletal pain and disability. Elsevier, Amsterdam, 2002.
- Malmivaara A, Hakkinen U, Aro T, et al. The treatment of acute low back pain - bed rest, exercises, or ordinary activity? N Engl J Med 1995;332:351-5.
- Manniche C, Lundberg E, Christensen I, et al. Intensive dynamic back exercises for chronic low back pain. Pain 1991;47:53-63.
- McGill S. The mechanics of torso flexion: situps and standing dynamic flexion manouvres. Clin Biomech 1995;10:184-192.
- McGill SM, Juker D, Kropf P. Quantitative intramuscular myolectric activity of the quadratus lumborum during a wide variety of tasks. Clin Biomechanics 1996;11(3);170-2.
- McGill SM. Low back exercises: evidence for improving exercise regimens. Physical Therapy 1998;78(7):754-764.
- McGill SM. Low Back Disorders: Evidence Based Prevention and Rehabilitation. Human Kinetics Publishers, Champaign, Illinois, 2002.
- McGill S, Grenier S, Bluhm M, et al. Previous history of LBP with work loss is related to lingering deficits in biomechanical, physiological, personal, psychosocial and motor control characteristics. Ergonomics 2003;46:731-746.
- McGill SM: Spine Instability. In: Liebenson, C (editor): Rehabilitation of the Spine: A Practitioner's Manual, 2nd ed., Baltimore, 2005 (sched pub) Lippincott Williams & Wilkins.
- O'Sullivan P, Twomey L, Allison G. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolysthesis. Spine 1997;24:2959-2967
- Richardson C, Jull G, Hides J, Hodges P. Therapeutic Exercise for Spinal Stabilization in Lower Back Pain, Churchill Livingstone, 1999.
- Snook SH, Webster BS, McGorry RW, et al. The reduction of chronic nonspecific low back pain through the control of early morning lumbar flexion. Spine 1998;23:2601-2607.
- Wilder DG, Aleksiev AR, Magnusson ML, et al. Muscular response to sudden load. A tool to evaluate fatigue and rehabilitation. Spine 1996; 21:2628-39.
Craig Liebenson, DC
Los Angeles, California
Click here for previous articles by Craig Liebenson, DC.