It should always be determined during consultation whether the patient's symptoms become worse with standing, running and other weight-bearing activities, regardless of the chief complaint.
If the foot is not functioning properly, extensor muscles of the pelvis may be giving inadequate support, which allows anterior pelvic rotation and increases the lumbar lordosis. In this case, the primary condition is foot dysfunction, even though the feet are asymptomatic. Treatment directed to the facet syndrome may well give relief, but if the basic underlying cause of the condition is not corrected, it will only be temporary.
One of the documented reasons for facet syndromes and lumbar hyperlordosis is inhibition of the gluteus maximus muscles.1 Fortunately, the gluteus maximus muscles can be tested in the prone, supine and standing positions.2 Immediate strengthening or weakening of the gluteus maximus muscles upon standing or after walking provides immediate, non-invasive evidence that foot dysfunction is related to the gluteus maximus muscle inhibition and related low back and pelvic problems. Two studies have shown that the gluteus maximus muscle was significantly delayed in activation in subjects following an ankle sprain injury compared to control groups.3-4
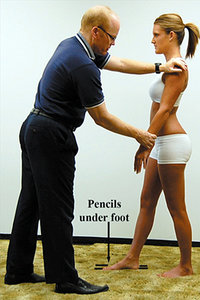 Pencils under the 1st and 5th metatarsals.
Knowledge of disturbance from the weight-bearing mechanism can be enhanced by determining if the patient feels better on arising in the morning, and the symptoms develop or increase with weight-bearing activity throughout the day. The weight-bearing mechanism is especially indicted if relief is obtained by sitting or lying down at the end of the workday.
Pencils under the 1st and 5th metatarsals.
Knowledge of disturbance from the weight-bearing mechanism can be enhanced by determining if the patient feels better on arising in the morning, and the symptoms develop or increase with weight-bearing activity throughout the day. The weight-bearing mechanism is especially indicted if relief is obtained by sitting or lying down at the end of the workday.
The afferent supply from the foot is instrumental in much of the organization of body movement and postural regulation. Many studies show that improper stimulation to proprioceptors disturbs the temporal pattern of muscle contraction, i.e., agonist and antagonist muscles contract at the same time; or there is contraction or inhibition not in keeping with the movement taking place at that time.5-7
Normal facilitation and inhibition of muscles can be demonstrated by manual muscle testing the shoulder flexors and extensors with an individual in various gait positions.8 When an individual is in a simulated gait position with the right leg forward and the left trailing, the left shoulder extensors test weak, despite being strong in a normal stance. This is expected in order for the arm to swing forward easily during that phase of gait.
However, if one places pencils under the first and fifth metatarsals (causing an artificially produced dropped metatarsal arch) the normal facilitation and inhibition of the shoulder muscles with various gait positions become unpredictable. It is not known how they will test, but in nearly all cases the results are different from the predictable norm.
During normal walking, there is alternate facilitation and inhibition of the sternocleidomastoid and upper trapezius muscles to keep the head pointed forward as the shoulder girdle rotates with the gait; otherwise, one's head would rotate with the shoulder girdle. The organization of these muscles relates to the input from the foot and ankle proprioceptors.9 Since the muscles insert into the skull, an improper temporal pattern can cause strain in the cranium and possibly create cranial dysfunctions.
Tecco, et al.,10 have also shown there are detectable interrelationships between occlusion and locomotion. It is not uncommon in chiropractic practice to observe loss of cranial corrections as soon as the patient walks or runs. The correction is usually maintained after a foot, gait or some other locomotion problem is corrected.
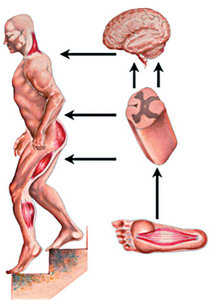 Afferent supply from the foot guides movement when standing.
As noted, shoulder motion harmony depends on proper inhibition and facilitation of the shoulder muscles, which are integrated with proper proprioception from the foot, leg and pelvis during walking.11 All patients with shoulder problems should have screening tests of the foot mechanism early in their evaluation. With recurrent or resistant shoulder problems, a thorough evaluation of the feet, legs and pelvis must be done.
Afferent supply from the foot guides movement when standing.
As noted, shoulder motion harmony depends on proper inhibition and facilitation of the shoulder muscles, which are integrated with proper proprioception from the foot, leg and pelvis during walking.11 All patients with shoulder problems should have screening tests of the foot mechanism early in their evaluation. With recurrent or resistant shoulder problems, a thorough evaluation of the feet, legs and pelvis must be done.
Improper stimulation to the proprioceptors of the joints, skin and muscles of the feet and legs can cause a bombardment of improper afferent impulses to the neuronal pools. This is especially true if there is a facilitated state at a spinal segment from a vertebral subluxation.12-13 The facilitated spinal neurons are initiated by afferent impulses arising from nociceptors or visceral receptors and are then transmitted to the dorsal horn of the spinal cord, where they synapse with interconnecting neurons. These stimuli are then transmitted to motor and sympathetic efferents, resulting in changes in the physical tissues, such as skeletal muscle, skin and blood vessels.
General structural strain throughout the body gives indication to evaluate the weight-bearing mechanism. Hammer, Rolf and Myers14-16 have pointed out the continuity of myofascia throughout the body, and how distortion in one area can transmit strain to remote body parts through the myofascia.
When there is structural strain, such as that present when the positive support reaction is not functioning adequately, the most superior aspect of the myofascia – at the crown of the head – is tense.2 Tenderness to digital pressure posterior to the bregma indicates probable myofascial tension.
Clinical evidence indicates that the pull of the myofascia around the skull can jam sutures.17 Especially important is the sagittal suture, which, when jammed, may cause weak abdominal muscles.18 The weak abdominal muscles allow the pelvis to rotate anteriorly, compounding the increased AP spinal curves from poor function of the positive support mechanism. It is possible that the abdominal muscle weakness correlates with a sagittal suture cranial dysfunction because the abdominal ptosis causes a generalized traction on the myofascia, which ultimately results in tightening of the superficial and deep myofascia of the epicranium. This could provide a vicious circle of cranial etiology that disturbs the function in such a manner that the cranial dysfunctions cause additional muscle weakness.
Another observation is the important role the abdominal muscles play in pelvic support, especially in category I pelvic dysfunction.19 The category I pelvic dysfunction is especially important in the cranial-sacral primary respiratory mechanism. Correcting the sutural dysfunction will very likely be only temporary unless other structural corrections are made, because the tense myofascia will cause the suture to jam again.
Recurrent cranial dysfunctions are body language to examine the weight-bearing and gait mechanisms. There are many reasons for this. Ferguson20 suggests that the powerful muscles attaching directly to the cranial bones are capable of generating sufficient pressure or forces upon the skull to produce the flexibility and palpable motion at the cranial sutures which may exist for this purpose. Just as it is imprudent to diagnose the status of the pelvic joints without knowledge of the status of the dynamic muscles which attach to the bones of the pelvis (such as the gluteus maximus, hamstrings, piriformis, quadratus lumborum or psoas), so must evaluation and treatment of cranial dysfunctions demand the evaluation of those muscles which attach to the skull.17
Page21 documents the continuity of the myofascia from the abdominal area to the dura mater. The deep cervical myofascia is so continuous with that of the head that the two should be considered as one. In addition, the deep cervical myofascia forms the pectoral myofascia, which in turn blends with the myofascial covering of the rectus abdominis.
Many times when there is a "rigid" skull on chiropractic examination, it relates with postural strain often associated with foot dysfunction. One can often feel greater rigidity of the skull when challenging an individual in the standing weight-bearing position than when sitting, supine, or prone. Before lasting corrections can be obtained in the stomatognathic or craniomandibular system, the structural strain from weight-bearing dysfunctions must be corrected.
An anterior cruciate ligament injury can produce changes in the masseter, anterior temporalis, posterior cervicals, upper and lower trapezius and sternocleidomastoid muscles.22 An increase in active mouth opening and a decrease in myofascial trigger point sensitivity in the masseter muscle were observed in response to the stretch of the hamstring muscles, demonstrating a functional relationship between the masticatory and hamstring muscles.23
Afferent supply from the feet is also instrumental in the organization of the sacrospinalis and other large muscles of the spine.24 Disorganization of these muscles can cause spinal or pelvic subluxations to recur as soon as the patient walks, even though they were adequately corrected.
During consultation, the presence of symptoms may be volunteered by the patient, but more often they are observed or "dug out" by the physician. One must often ask leading questions that can be analyzed by the physician's knowledge of body integration.
References
- Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual: The Lower Extremities. Williams & Wilkins: Baltimore; 1992.
- Cuthbert S. Applied Kinesiology: Clinical Techniques for Lower Body Dysfunctions; 2013. https://www.thegangasaspress.com.
- Bullock-Saxton JE, Janda V, Bullock MI. The influence of ankle sprain injury on muscle activation during hip extension. Int J Sports Med, 1994;15(6):330-4.
- Bullock-Saxton JE. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther, 1994;74(1):17-28.
- Gardner-Morse MG, Stokes IA. The effects of abdominal muscle coactivation on lumbar spine stability. Spine, 1998;23(1):86-91; discussion 91-2.
- Graven-Nielsen T, Svensson P, Arendt-Nielsen L. Effects of experimental muscle pain on muscle activity and co-ordination during static and dynamic motor function. Electroencephalogr Clin Neurophysiol, 1997;105(2):156-64.
- Bard C, Paillard J, Lajoie Y, Fleury M, Teasdale N, Forget R, Lamarre Y. Role of afferent information in the timing of motor commands: a comparative study with a deafferented patient. Neuropsychologia, 1992;30(2):201-6.
- Goodheart GJ, Jr. Applied Kinesiology Research Manuals. ICAKUSA: Shawnee Mission, KS; 1982.
- Dananberg H. Lower Back Pain as a Gait-Related Repetitive Motion Injury. In: Vleeming A, et al. (Eds.) Movement, Stability and Low Back Pain. New York, NY: Churchill Livingstone;2007:253-264.
- Tecco S, Salini V, Calvisi V, Colucci C, Orso CA, Festa F, D'Attilio M. Effects of anterior cruciate ligament (ACL) injury on postural control and muscle activity of head, neck and trunk muscles. J Oral Rehabil, 2006;33(8):576-87.
- Geyer H, Herr H. A muscle-reflex model that encodes principles of legged mechanics produces human walking dynamics and muscle activities. IEEE Trans Neural Syst Rehabil Eng, 2010;18(3):263-73.
- Leach RA. The Chiropractic Theories: Principles and Clinical Applications, 3rd Edition. Williams & Wilkins: Baltimore; 1994:89-115.
- Korr IM. The spinal cord as organizer of disease processes: some preliminary perspectives. JAOA, 1976;76(1):35-45.
- Hammer W. "Fascial Thickening Is Responsible for Musculoskeletal Pain." Dynamic Chiropractic, May 20, 2012.
- Myers TW. Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists. Churchill-Livingstone; 2001.
- Rolf IP. Rolfing: The Integration of Human Structures. Dennis-Landman Publishers: Santa Monica; 1977.
- Chaitow L, et al. Cranial Manipulation – Theory and Practice: Osseous and Soft Tissue Approaches, 2nd Edition. Elsevier: Edinburgh; 2005: 241-254.
- Walther DS. Applied Kinesiology, Volume II - Head, Neck and Jaw Pain in Dysfunction-The Stomatognathic System. Systems DC: Pueblo, CO; 1983.
- Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. Spine, 1996;21(22):2640-2650.
- Ferguson A. Cranial osteopathy: a new perspective. J Acad Appl Osteo, 1991;1(4):12-16.
- Page LE. The role of the fasciae in the maintenance of structural integrity. Acad Appl Osteo Yr Bk, 1952.
- Tecco S, Polimeni A, Saccucci M, Festa F. Postural loads during walking after an imbalance of occlusion created with unilateral cotton rolls. BMC Research Notes, 2010;3:141.
- Fernández-de-las-Peñas C , Carratalá-Tejada M , Luna-Oliva L, Miangolarra-Page JC. The immediate effect of hamstring muscle stretching in subjects' trigger points in the masseter muscle. J Musculoskel Pain, 2006;14:27-35.
- Kavounoudias A, Roll R, Roll JP. Foot sole and ankle muscle inputs contribute jointly to human erect posture regulation. J Physiol, 2001;532(Pt 3):869-78.
Dr. Scott Cuthbert is the author of Applied Kinesiology Essentials: The Missing Link in Health Care (2013), and Applied Kinesiology: Clinical Techniques for Lower Body Dysfunctions (2013), the content of which forms the basis for this and subsequent articles. Dr. Cuthbert is a 1997 graduate of Palmer Chiropractic College (Davenport) and practices in Pueblo, Colo. He has published Index Medicus clinical outcome studies and literature reviews, and 50 peer-reviewed articles on chiropractic approaches.




