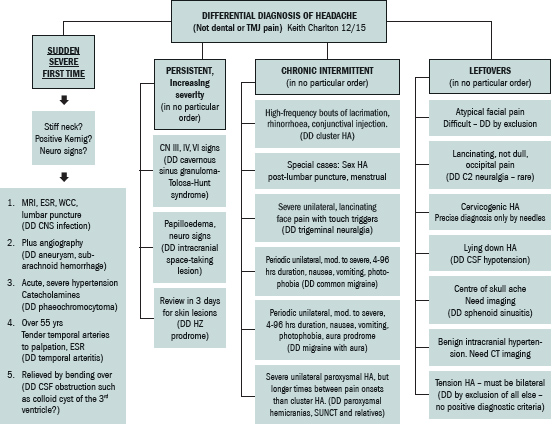
Chiropractors frequently see patients with headaches and frequently successfully provide relief, but despite many tomes on the subject of headache,1-8 there seems to be little helpful data on differential diagnosis that permits construction of an easy algorithm for those of us in clinical practice.
A. Pain, referred from a source in the neck and perceived in one or more regions of the head and/or face, fulfilling criteria C and D [below].
B. Clinical, laboratory and/or imaging evidence of a disorder or lesion within the cervical spine or soft tissues of the neck known to be, or generally accepted as, a valid cause of headache.
 C. Evidence that the pain can be attributed to the neck disorder or lesion based on at least one of the following:
C. Evidence that the pain can be attributed to the neck disorder or lesion based on at least one of the following:
- Demonstration of clinical signs that implicate a source of pain in the neck
- Abolition of headache following diagnostic blockade of a cervical structure or its nerve supply using placebo or other adequate controls
D. Pain resolves within three months after successful treatment of the causative disorder or lesion.
Even these guidelines deny a role for clinical diagnosis of cervicogenic headache. Objective confirmatory tests are lacking, too invasive or not generally available. Disorders of the upper cervical spine are implicated as a headache cause by virtue of the anatomy of the region16 and by a controlled study17 that demonstrated headaches stemming from the C2-3 zygapophysial joint could be identified by diagnostic blocks of the third occipital nerve innervating the joint.
Two authors18 propose a pragmatic diagnostic approach to probable cervicogenic headache with a list of seven clinical criteria, as well as a "rigorous approach to the diagnosis and management of definite cervical headache," such as percutaneous radiofrequency neurotomy.
Since clarity leads to power, I have mentally tossed around diagnostic options for trying to achieve such an algorithm and come up with one for me. Maybe you can work out one for yourself (or use what I've come up with). As always, thanks for thinkin' with me!
References
- McGrath PA, Hillier LM (eds). The Child With Headache: Diagnosis and Treatment. Seattle: IASP Press, 2001.
- Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 2nd Edition. Cephalalgia, 2004; (Supplement 1);24:115-17.
- Bogduk N, Corrigan B, Kelly P, Schneider G, Farr R. Cervical headache. Med J Aust, 1985;143:202-7.
- Goadsby PJ. Cervicogenic headache: a pain in the neck for some neurologists? Lancet Neurology, 2009;8:875-8.
- Bogduk N, Corrigan B, et al., Op Cit.
- Lord SM, Barnsley J, Wallis BJ, Bogduk N. Third occipital headache: a prevalence study. J Neurol Neurosurg Psychiatry, 1994;57:1187-90.
- Olesen J, Goadsby PJ, Ramadan NM, Tfelt-Hansen P, Welch KMA. The Headaches, 3rd Edition. Philadelphia: Lippincott Williams & Wilkins, 2010.
- Baron R, May A. Headache and Pain. Washington D.C.: IASP Press, 2014.
- Headache Classification Committee, Op Cit.
- Bogduk N, Corrigan B, et al., Op Cit.
- Bogduk N, Marsland A. On the concept of the third occipital headache. J Neurol Neurosurg Psychiatry, 1986;49:775-80.
- Bogduk N. Cervical causes of headache. Cephalalgia, 1989;9 (Suppl 10):172-3.
- Antonaci F, Fredricksen TA, Sjaastad O. Cervicogenic headache: clinical presentation, diagnostic criteria, and differential diagnosis. Curr Pain Headache Rep, 2001;5:387-92.
- Antonaci F, Ghirmai S, Bono G, Sandrini G, Nappi G. Cervicogenic headache: evaluation of the original diagnostic criteria. Cephalalgia, 2001;21:573-83.
- Goadsby PJ. Cervicogenic headache: a pain in the neck for some neurologists? Lancet Neurology, 2009;8:875-8.
- Bogduk N, Marsland A, Op Cit.
- Lord SM, et al., Op Cit.
- Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurology, 2009;8:959-68.
Dr. Keith Charlton, a 1975 graduate of National College of Chiropractic, practices in Brisbane, Queensland (Australia). Over the years, he has held membership in various chiropractic associations and been active on a political level, including serving as president of the Queensland Branch of the Chiropractors' Association of Australia, during which time he helped secure legislative recognition for the profession in Queensland. He is a member of the editorial boards of Chiropractic & Osteopathy and the Journal of Chiropractic Humanities, and previously served on the boards of several other peer-reviewed journals including JMPT and the Chiropractic Journal of Australia.




