Have you encountered patients with groin and hip pain you can't seem to solve? You know it's not a worn-out hip; you suspect the pain is somehow connected to the spine. But somehow, you just can't help them break through.
I think the thoracolumbar area (TL), and the peripheral sensory nerves that exit here, are important and rarely recognized sources of lower back and pelvic pain. My previous article in DC1 and articles on my website2 have focused on the posterior components.
This article was inspired by a young, athletic female patient who came to me after a year of hip and groin pain. She had gone to a great PT before she saw me. She was faithfully doing quality rehab; I had adjusted her hip, and it was moving somewhat better. I had adjusted her TL, aiming at normalizing the peripheral nerves via that approach.
Despite all this, she still was having lateral hip pain and groin pain. This woman, who previously could run long distances, could not even walk without pain. Despite all of our work, she was not much better. On exam, she still showed tenderness over the exit points of the ilio-hypogastric nerve and the lateral femoral cutaneous nerve. That ongoing finding led me to further exploration of other possible lumbar nerve impingement sources. She finally responded after I began using this abdominal release work.
Anterior Lumbar Nerves: Anatomy
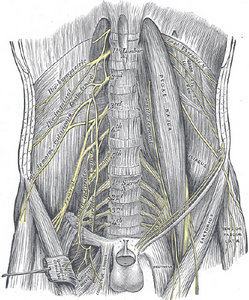 Anterior lumbar nerves at the back wall of the abdomen. Note the oblique lateral course of ilio-hypogastric and ilio-inguinal nerves, and the more inferior course of the obturator and genito-femoral nerve.
Let's start by reviewing the relevant anatomy. Where do the nerves begin, what is their course,and what area do they supply? We will need a palpable superficial tender point to guide our clinical assessment protocol (CAP).
Anterior lumbar nerves at the back wall of the abdomen. Note the oblique lateral course of ilio-hypogastric and ilio-inguinal nerves, and the more inferior course of the obturator and genito-femoral nerve.
Let's start by reviewing the relevant anatomy. Where do the nerves begin, what is their course,and what area do they supply? We will need a palpable superficial tender point to guide our clinical assessment protocol (CAP).
The ilio-hypogastric and ilio-inguinal nerves (L1) initially run obliquely laterally and then curve through the posterior soft tissues, exiting via the lateral groin and hip. The genito-femoral (L1-2) and obturator nerves (L2-4) run more vertically down into the groin.
The lateral branch of the ilio-hypogastric exits just above the iliac crest and supplies the skin over the gluteal area. Its tender point is at the top of the gluteus medius, more or less along the lateral line.
The ilio-inguinal nerve continues to descend through the medial part of the groin, and supplies sensation to the medial thigh and the genital organs. (I am less clear on exactly where to palpate its tender points.)
The genito-femoral nerves (L1-2) and the obturator nerves (L2-L4) have a more vertical course, and supply both the anterior thigh and the genital organs. When the obturator nerve is irritated, the obturator foramen will be tender.
L2 is the origin of the lateral femoral cutaneous nerve, which initially travels obliquely lateral and inferior, and has two branches. The anterior branch supplies the anterolateral thigh; the posterior one supplies the skin from the greater trochanter down to the knee. The tender point is just medial to the ASIS, within the iliacus muscle. There is some variability in the origin of these nerves, coming from T12 to L3.3
Examination Tips
How can you assess these peripheral sensory nerves? (These are peripheral sensory nerves primarily, and some have motor function.) Why are these specific points tender? The hypothesis is that these nerves are irritated, both at the spine and along their course. At specific areas, there is further irritation due to their passage through a narrow place. Our indicators on palpation will be tenderness and mild swelling.
Lets focus on two key tender nerve points that have an anterior origin. The first one is the ilio-hypogastric nerve at the top of the gluteus medius, just below the iliac crest, on the lateral line. The second is the lateral femoral cutaneous nerve, just medial to the ASIS.
When a sensory nerve is irritated and creates pain, the corresponding muscles often become weak and inhibited secondary to the pain. Muscle testing / functional testing of the involved areas may give us additional useful information. To complete this exam, examine the spine for restriction and tenderness of the joints of the thoracolumbar junction.
 Location (noted by dot) of the exit point of the iliohypogastric
Location (noted by dot) of the exit point of the iliohypogastric
nerve.
How can you palpate these nerve exit points? Start with the patient either sitting in front of you or prone. Touch directly on the skin (the patient can just pull their shirt up and their pants a little ways down) just below the iliac crest. This area just below the iliac crest gives us critical information which guides the rest of the assessment and treatment.
For the complete exam of these TL peripheral nerves, start medially, just lateral to the PSIS, and work your way around laterally. Eventually, you will turn the patient supine to get a better sense of the lateral femoral cutaneous point, and to access the groin and abdomen. Use these tender points as your indicators both before and after treatment.
I always use a skin pencil to mark the tender points, so the patient and I really know we are on the right spot. In many cases, there also will be tenderness and mild swelling in multiple locations along the nerve course.
When Should You Check the Nerves?
What clinical complaints would make us assess these lateral and anterior tender nerve points, and their upstream sources? I've already mentioned lower back or pelvic pain. Others include lateral or anterior hip pain, groin and/or genital area pain, especially when these are not responding to your adjustments and rehab.
The lateral femoral cutaneous nerve, when it is impinged, is the cause of meralgia paresthetica. When the patient has anterior thigh pain or sensory changes, don't forget the simpler causes. Patients can't get well if they are doing something that is directly irritating the nerve, over and over. To quote William Morgan, DC: "The simplest treatment for any condition is to take away the cause. If the patient is wearing tight clothes, belts, load-bearing belts, then those should be removed. If the patient is obese, then weight loss would be the primary treatment."4
Evaluating & Treating Abdominal Fascia to Release the Nerves
For treatment, the patient should be supine with their knees bent and supported over a pillow. Begin by palpating along the course of the psoas. I take an anterior approach to this muscle. I have noticed that the psoas usually has one or more specific segmental levels of restriction and tenderness. This correlates with the psoas nerve supply, which is segmental. I begin by using gentle myofascial work to release the specific levels of the psoas that feel "tight."
Once the psoas begins to release, I follow the lines of the nerves. The ilio-hypogastric and lateral femoral cutaneous exit laterally to the psoas, and travel along the posterior abdominal wall. The ilio-inguinal, genito-femoral and obturator travel along a more vertical path. Can I be sure I am on the exact nerve in question? I am not quite sure. I do know when I am feeling fascia that does not quite feel right.
I am doing gentle fascial release, aimed along the course of the involved nerves. At times, I am directly following the nerve pathways; at other times, I am doing fascial release in the area of these nerves. This is where the written word is inadequate. If I am successful, when I am done, the previously tender iliac crest points will be substantially diminished.
If you were to look at my hands when I am doing this work, they are not 4 inches deep in the abdomen. Visceral manipulation and my training in osteopathic techniques have taught me how to be subtler in my approach to the abdomen. My hands and fingers are flat, not pointed down toward the spine. I am sinking into the abdomen and feeling through the fluid medium of the abdominal organs.
In executing this specific technique, I am not that interested in the organs. I am interested in the nerves that are on the posterior abdominal wall, deep to the organs, behind the peritoneum.
I want to remind you to put on your "gentle mode" hat when you do this work. It is not Rolfing, it is not deep tissue, it is not Graston, it is not active release. It is gentle fascial work, more similar to craniosacral, Barnes myofascial work or visceral manipulation.
Rehab Exercises
Now let's address rehab exercises for this region. What stresses the TL area? In my simple mind, the problem is excessive lateral bending and/or excessive TL extension. I used to think my patients could stretch out of this pain, but I am convinced the better rehab strategy for most tight areas lies in activating the proper muscles. We attempt to address the core, with focus on breath, the oblique abdominals and the QL area. The glutes, especially the gluteus medius, can be critical.
When the gluteus medius is weak, the patient's gait changes. Especially if they are more mobile, they go into a Trendelenberg-type gait (think of a classic woman's "swish" of the behind). If they are leaking out to the side every time their foot strikes, they are putting a lateral stress on the TL area. This can reproduce the same nerve pain pattern.
You can use a fairly basic rehab strategy: side planks, side plank plus when the hip is involved, and various gluteal-awakening strategies. DNS and PRI rehab both focus on getting the diaphragm properly lined up, and correcting an excessive thoracolumbar hinge pattern through proper breathing and proper firing of the abdominals.
The goal with this entire discussion is to give you another tool to address some of your more difficult patients. I hope my descriptions give you enough information to get started. Your initial database is probably small. Palpate more abdomens and you will begin to develop these skills. The bottom line: The more patients you can help, the better.
References
- Heller M. "How to Fix and Find TL Nerve Impingements." Dynamic Chiropractic, April 15, 2015.
- For more information on the TL junction and its nerves, read the articles on my website: http://sosas.us/professional-resources/articles-2/.
- Bergman RA, Afifi AK, Miyauchi R.Illustrated Encyclopedia of Human Anatomic Variation: Opus III: Nervous System Variations in Formation of Ilioinguinal Nerve.
- Morgan W. "Meralgia Paresthetica: Skinny Jeans Syndrome." Clinicians Corner: Lumbo-Pelvic Series, Part 3.
Click here for more information about Marc Heller, DC.





