Pelvic pain is a common complaint. The problem is of increasing significance and may be a direct result of contemporary lifestyles, which include spending a lot of time at desks and/or in front of computers.
Most people rarely partake in even a minimal amount of stretching exercises designed to lengthen taut, shortened tissues and loosen joints. Add to that a general lack of exercise, poor diet and an overall increase in Americans' weight. With 61 percent of the population overweight (27 percent of whom have been diagnosed as clinically obese), it shouldn't be a surprise that this degree of increased weight causes more stress and strain on the pelvis and those articulations used when standing, walking and running.1
Patients also expose themselves to a variety of traumas that often do not heal properly, leading to osteoarthritis, fibrotic joint capsules, and myofascial trigger points. Chronic pelvic pain is the cause of more than $2.8 billion in annual outpatient spending.2
Pelvic Anatomy and Pain Patterns
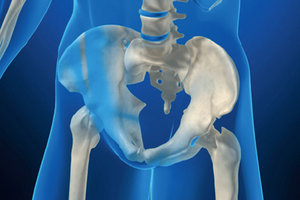
The pelvis resembles a hollow container – or "basin" – filled with viscera. One of its primary functions is to allow the egress and ingress of neurovascular and muscular structures. The pelvis consists of three articulating structures that form a three-joint complex. The sacrum is a triangular bone wedged between the posterior aspects of the two innominate bones at the sacroiliac joints. The innominates meet anteriorly at the pubic symphysis.3
 Any discussion of pelvic pain is usually separated into two main categories. Mechanical disorders of the lower back, hip, and sacroiliac joints can cause pain in the pelvis. Organic dysfunctions of the bowel and bladder, and gynecologic disorders can also cause pain in the pelvis. Often the patient is not able to tell if the cause of pain is organic, or if it was induced by a mechanical problem as a result of an accident or a lifting incident. Some of the common organic dysfunctions causing pelvic pain include dysmenorrhea, endometriosis, prostatitis, renal stones, rheumatoid arthritis, osteoporosis, hernia, and tumors.
Any discussion of pelvic pain is usually separated into two main categories. Mechanical disorders of the lower back, hip, and sacroiliac joints can cause pain in the pelvis. Organic dysfunctions of the bowel and bladder, and gynecologic disorders can also cause pain in the pelvis. Often the patient is not able to tell if the cause of pain is organic, or if it was induced by a mechanical problem as a result of an accident or a lifting incident. Some of the common organic dysfunctions causing pelvic pain include dysmenorrhea, endometriosis, prostatitis, renal stones, rheumatoid arthritis, osteoporosis, hernia, and tumors.
Deep pelvic pain is frightening to many patients since it mimics the pain of a diseased organ. In cases of this type, the patient usually consults a medical physician, who may not understand the role of somatic pain referral. The first thing the physician may do is perform a laparoscopy to rule out visceral pathology. It is estimated that up to 75 percent of exploratory laparoscopies for pelvic pain reveal normal tissue. The problem with a normal laparoscopy finding is that the patient is often then assumed to have a psychiatric problem. (It is imperative that doctors of chiropractic advise patients who require a referral to get a proper one – not only for the patients' sake, but also to keep from having to defend their actions in court.)
Examination and Treatment
On a patient's initial visit, several important factors can help pinpoint an accurate diagnosis. First, a carefully taken history is imperative and should include details of the patient's activities of daily living, medical history, diet and exercise. Next, make sure your exam is thorough; do not cut corners. There are many orthopedic tests for the low back and pelvis that help differentiate the nature of the problem. In addition, ranges of motion, palpation of the abdomen, and simple things such as a kidney punch test are important to document. A lack of any positive orthopedic tests and good ranges of motion may suggest that you should look for some type of organic dysfunction.
If you don't already use one of the accepted pain assessment instruments, such as the Pain Disability Index (PDI), the Beck Depression Inventory or the RAND-36 Health Survey, you may want to start. They will help demonstrate progress when combined with all other objective tests. This standard of practice also includes appropriate X-rays to help rule out tumors, stones and of course, fractures.
Motor-vehicle accidents and falls from a significant height are the leading causes of pelvic fractures. There have also been cases of pelvic stress fractures found in runners who have been in training for a marathon or may have simply increased the distance they are running. Unfortunately , an X-ray doesn't always pick up subtle fractures. When you feel it is appropriate, get an MRI or have a bone scan done.
A research study at Palmer College of Chiropractic examined subjects who complained of chronic pelvic pain for a median duration of nine years and a range of 1-25 years. The subjects were enrolled in chiropractic care, which included adjustments using flexion-distraction technique and manual trigger-point therapy. Before the study began, two-thirds of the subjects reported frequent use of analgesics.
By the end of the study, half had stopped using them. Several reported having pain-free intercourse for the first time. Others said that they had a decrease in menstrual cramping as the study progressed. This study concluded that the use of flexion-distraction technique and manual trigger-point therapy had positive short-term effects on symptomatology, disability and pain associated with chronic pelvic pain.2
A study done at National College of Chiropractic took subjects with mechanically induced pelvic pain and others with organic dysfunction pelvic pain and put them through a care plan using a modified Cox technique, electric muscle stimulation and cryotherapy. Their results again supported the use of chiropractic management in the care of pelvic pain of both mechanical and organic nature.4
Surgical scars have been recognized as a source of local and referred pain. For example, surgical scars on the abdomen are known to refer pain to the lower back, sacroiliac joints, and into the deep regions of the pelvis. To evaluate the scar, have the patient run a finger along the scar, applying moderate pressure, or roll the scar between the thumb and index finger. If painful trigger zones are found or if a loss of mobility is noted in the involved tissues, a course of myofascial release technique would benefit the patient and could release the source of the patient's pelvic, sacroiliac or lower-back pain.5
Specific chiropractic adjustments to the pelvis restore joint play at dysfunctional joints, relax hypertonic muscles, and disrupt articular and periarticular adhesions.6 Treatment of myofascial trigger points is also effective in many patients who suffer from the shortening of certain muscles as a result of activities of daily living. Stretching and strengthening of specific muscle groups will also increase the effectiveness of chiropractic adjustments and myofascial therapy.
Once the pelvis has been adjusted, the trigger points worked out and the muscles stretched, it may be beneficial to stabilize your work by using individually designed stabilizing orthotics for the feet. Orthotics used on a pronated foot can decrease the quadriceps femoris muscle angle or Q angle.7
In a standing position, this angle is determined by drawing a line from the anterior superior iliac spine to the center of the patella. A second line is drawn from the center of the patella to the tibial tubercle.8 A decreased Q angle will put less pressure on the quadriceps and will, in turn, take pressure off the knee and hip joints.
The pelvis is complex in the fact that there are so many muscles that attach to it, along with many neurovascular structures which enter and exit from it. Fortunately, research suggests chiropractic adjustments and adjunctive care can be effective treatment strategies.
References
- Pilzer PZ. The Next Trillion. Dallas, TX: Video Plus Inc., 2001:5.
- Azad A, Long C, Hawk C, Cox JM. Chiropractic care for women with chronic pelvic pain. Alt Ther Health & Med, 1997;3(2):91.
- DeFranca GG. Pelvic Locomotor Dysfunction: A Clinical Approach. Gaithersburg, MD: Aspen Pub., 1996:1.
- Browning J. Distractive manipulation protocols in the treating of mechanically induced pelvic pain and organic dysfunction patient. J Manip Physiol Ther, 1995;18(12):644.
- Culp V. Surgical scars and their link to chronic abdominal and lower back pain. Chiro J, 1994;9(3):40.
- DeFranca, Op Cit, page 290.
- D'Amico JC, Rubin M. The influence of foot orthotics on the quadriceps angle. J Am Pod Med Assn, 1986;76:337-340.
- Weinstein ST, Buckwalter JA, editors. Turek's Orthopaedics: Principles and Their Application, 6th Edition. Philadelphia: Lippincott Williams & Wilkins, 1995.
Click here for previous articles by Mark Charrette, DC.





