In this article, you'll learn about patterns of chronic dysfunction that occur secondary to ankle sprains. This is not about the acute ankle sprain; the working assumption here is that the injury occurred long ago and left the patient with some degree of damage.
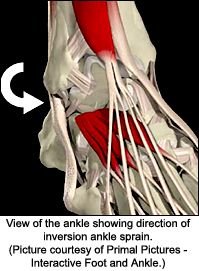
Inversion Ankle Sprain Patterns
In a typical inversion ankle sprain, the foot is suddenly inverted, straining the lateral ligaments and leading to an inferior motion of the fibula. This motion often leads to a fibula stuck anterior and inferior.1 This can be accessed through palpation of the inferior portion of the lateral malleolus, which will be tender and resist the testing motion. You can correct this with recoil, or engage, listen, follow (ELF), or use instrument adjusting.
You also need to check the talus, as well as the cuboid and fifth metatarsal. Aberrant mechanics of the lateral ankle and foot are consistent with the motion that occurs in the inversion sprain, whereby the ankle supinates. The foot and ankle will often be stuck in this supinated position. Don't think dropped cuboid; think supinated cuboid. Don't think lateral talus; think supinated talus. This visualization will give you a clearer picture of the usual three-dimensional mechanics. Use your palpation skills to fine-tune your adjustment.
Ligaments that need addressing here could include any of the lateral ligaments. Check the anterior and/or posterior talofibular ligaments, as well as the calcaneofibular ligament. You should also check the anterior tibiofibular ligament. Treatment of old ligaments injuries is addressed below. The muscles should be checked, especially the lateral ones, including the peroneal muscles, the biceps femoris, and the gluteus medius.
Functional Diastasis of the Ankle Mortise
A significant lesion at the ankle involves a functional diastasis between the fibula and tibia. This is often seen after a classic inversion sprain. This can also be a sequela of the high ankle sprain, usually caused by dorsiflexion combined with external rotation of the foot. This is a less common sprain and involves the opposite motion, eversion. An excellent recent review of high ankle sprain diagnosis and treatment is referenced at the end of this article.2 A diastasis, or grade three sprain, is usually defined as a pathological separation between two bones. Far more often, the separation is not obvious on X-ray and is not to the same degree as a pathological diastasis. The lesion I am describing is not a complete dislocation. It could be described as a functional diastasis.
Paul Chauffour (mechanical link therapy) describes these occurring at the distal tibia-fibula junction, at the pubic symphysis, and at the sacroiliac joint.3 At the distal tibia-fibula junction, this can involve a chronic sprain or tear of the extensor retinaculum, a thick band of deep fascia overlying the distal part of the anterior lower leg. You'll also find possible stretching and laxity of the interosseous ligament and/or the anterior and posterior tibiofibular ligaments (the syndesmotic ligament complex). The lateral ankle ligaments can also be involved. If the tibia and fibula are functionally separated here, the ankle and foot cannot function normally, leading to recurrent ankle sprains, foot or ankle pain, or problems further up the kinetic chain in the knee or lower back.
Your assessment here could start by evaluating the overall mobility of the ankle. It will usually feel somewhat "sloppy" with excessive mobility as you move it into inversion and/or eversion. I'll reference Ted Forcum, DC, for further orthopedic tests of these ligaments: The side-to-side test is for the integrity of the inferior tibiofibular ligaments and the interosseous membrane. The ankle is held in neutral position, without inverting or everting the calcaneus, while the foot is sheared transversely. A soft end-feel and excessive glide are positive findings. A positive test can frequently be associated with fracture. The external rotation stress test holds the ankle joint in neutral while externally rotating the foot. This tests the syndesmosis. The squeeze test is done by grasping the distal tibia and fibula and squeezing them together. The reduction of pain or excess excursion may indicate disruption of the syndesmosis.4
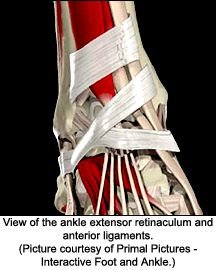 Palpation of these ligaments will reveal tenderness and possibly a slight bogginess, especially at their junctions with the bones. Damaged ligaments have a slight excessive "give" on palpation, although this is a subtle finding. Move more proximally and palpate the interosseous membrane, deep to the peroneal muscles, between the fibula and the tibia.
Palpation of these ligaments will reveal tenderness and possibly a slight bogginess, especially at their junctions with the bones. Damaged ligaments have a slight excessive "give" on palpation, although this is a subtle finding. Move more proximally and palpate the interosseous membrane, deep to the peroneal muscles, between the fibula and the tibia.
Assess the joints of the foot and ankle for restriction, and adjust accordingly. The pattern of dysfunction after the inversion sprain is described above. A high ankle sprain is a pronation event; thus, it will have different biomechanics, and need different adjusting corrections. The fibula and/or tibia may show intraosseous (within the bone) restrictions.5
Assess the muscles that surround the area, both by testing for strength and pain on contraction, and by looking for tenderness and/or tissue texture changes along the course of the muscles. The biceps femoris and gluteus medius are more proximal muscles that are often inhibited whenever the fibula is involved.6 Muscle involvement can include inhibition (weakness) and/or tightness, trigger points, and tendon insertionopathies. Muscular rehabilitation for the ankle would involve a focus on improving gait, and on retraining for speed and strength of contraction. Balance is key here, and can be enhanced by use of a wobble board, Czech balance sandals, or similar tools.
It is more difficult to use palpation to assess directly for ligamentous laxity if the distal tibia is functionally separated from the fibula. Besides the orthopedic tests described previously, you can use applied kinesiology-style "challenge" muscle testing.7 Use one hand to push the distal tibia and fibula apart, and then test an indicator muscle. Induced weakness would be another indication of functional separation. Another AK-type test would be to take your fist and "hammer" on the calcaneus, with the thump in a superior direction. This mild trauma will often produce weakness in an indicator when the ankle joint is dysfunctional.
You can use palpation to assess for a manipulable lesion here, where the distal fibula and distal tibia are stuck apart. Surround the ankle mortise with both of your hands, and push your hands toward each other. For the right ankle, stand or sit facing the patient and use the heel of your left hand to push the lateral malleolus toward the midline. Your right hand pushes the medial malleolus toward your left hand. You are feeling for restriction. This is a slightly different feel than your usual joint palpation; it will probably take you several repetitions on different patients to get a sense of this. Fine-tune the exact direction of push to find the maximum resistance point, and correct with recoil or ELF. The goal of the adjustment is to reset mechanoreceptors and address hypomobility.
Inherent in the concept of functional diastasis is instability with potential hypermobility or laxity - in this case, of the deep ligaments and fascia of the ankle mortise. Adjusting the hypomobility, and "resetting" is not usually enough. How can you address the instability?
I always do a simple taping afterward to help stabilize the ankle mortise. I take one piece of 1.5-inch or 2-inch nonelastic tape and apply it all the way around the lower leg just above the malleoli. I have the patient take a roll of tape home and retape the leg daily for six weeks or so. I recheck the patient periodically. If the patient cannot tolerate tape, instruct him or her to use a cloth band. The one I use is a basic cloth wrap with Velcro, designed for the wrist or elbow. Elastic tape or an elastic wrap is not as effective; you need to stop the ankle mortise from separating during gait. If the patient is a pronator or supinator, an orthotic used in good shoes will be necessary.
The ligaments and fascia of the region have usually been stretched in the original injuries that occurred here. Soft-tissue therapy is necessary to attempt to restart the early stages of the healing process. Let's define "healing" for these tissues more rigorously. First-stage healing is defined here as the process that occurs after an injury, involving inflammation, laying down of fibroblasts, and remodeling. Healing of this type takes 6-8 weeks, and basically stops after a certain amount of time, whether the ligaments and fascia are completely healed or not. The patients you see with chronic functional instability at the ankle are probably far beyond this stage of healing.
How can you help restart this process and retighten the ligaments? Here are three possible ways: One is Graston instrument-assisted soft-tissue mobilization. Davidson, et al., found that controlled microtrauma, induced through the Graston technique protocol, increased the amount of fibroblast production in the Achilles tendon of rats.8 The theory is that the structure of the tissue is rearranged, and damaged tissue is replaced by new tissue. Warren Hammer reviewed the research and clinical rationale for use of this modality in this publication.9 Another similar tool is cross-frictional massage. A third is proliferant injections, a medical procedure of injecting irritant solutions, including glucose, into the damaged ligaments. The goal of all three of these therapies is to restart the inflammation/healing cycle.
My own experience with these may be instructive. I have referred to colleagues using prolotherapy for at least 10 years. It has often been dramatically effective on old injuries, especially when I could not stabilize the patient. I tried cross-frictional massage after taking soft-tissue courses 15 years ago. I found it very time consuming and very hard on my hands, so I stopped using it. I recently took a Graston technique course, and I am excited to have this new, relatively easy-to-use modality, which allows me to both release fascial restrictions and restart the ligamentous/fascial healing process in an effective and quick manner.
I have attempted to share a comprehensive model of how to address chronic instability of the ankle mortise. Adjust the foot, the ankle, and the fibula and tibia. Adjust the separated tib-fib, if it is stuck apart. Address the surrounding ligaments and other soft tissues, ideally using methods such as Graston or cross-friction, which will enhance fibroblastic activity and restart first-stage healing. Tape the ankle mortise and use orthotics if necessary to stabilize during healing. Teach the patient to strengthen his or her foot and ankle muscles.
References
- Thomas M. Lower Extremity Manipulation courses, 2001-2002.
- Smith A, Bach B. High ankle sprains: minimizing the frustration of a prolonged recovery: The Physician and Sportsmedicine, December 2004;32(12): www.physsportsmed.com/issues/2004/1204/bach.htm.
- Chauffour P. Mechanical Link. North Atlantic Press, 2002.
- Forcum Ted, writing in Conservative Management of Sports Injuries (Hazel R, Hyde T, Gengenbach M, editors). Lippincott Williams & Wilkins, 1996.
- Heller M. Intraosseous restrictions. Dynamic Chiropractic, Nov 5. 2001: www.chiroweb.com/archives/19/23/12.html.
- Mark Thomas, DC, clinical conversations.
- Walther DS. Applied Kinesiology, Vol. 1, Basic Procedures and Muscle Testing. Systems DC, Pueblo, CO, 1988: pp. 25-26.
- Davidson CJ, Ganion L, Gehlsen G, et al. Morphologic and functional changes in rat Achilles tendon following collagenase injury and GASTM. Journal of the American College of Sports Medicine 1995;27(5).
- Hammer W. Graston instrument-assisted soft-tissue mobilization: a scientific and clinical perspective. Dynamic Chiropractic, May 20, 2004: www.chiroweb.com/archives/22/11/07.html.
Click here for more information about Marc Heller, DC.