Five stages of facet joint degeneration have been described pathologically: synovitis; joint capsule laxity; articular cartilage destruction; subarticular erosions; and hyperostosis. This pathologic classification is not easily observed radiographically, and even when utilizing computed tomography (CT) and magnetic resonance (MR) scanning, every stage is not detectable. However, it is helpful to keep these different stages in mind when evaluating a facet joint.
The first and second stages are not easily evaluated with present-day imaging procedures. The first stage, characterized by hyperemia and inflammatory cell infiltration within the synovium and the capsule of the facet joint, presently can be visualized only by direct biopsy examination of the synovium.
The second stage of degeneration, indicated by laxity of the joint capsule, also is not radiographically observable (with the possible exception of motion studies, which are difficult to evaluate, especially in the lumbar spine). This second stage may be suggested by biomechanical changes on the plain films such as in overriding of the facets. I believe that what we often see on plain films (such as the facet imbrication demonstrated by the Macnab's joint body line, the facet syndrome angle, the sacral base angle and the like) is this second stage, which often does not demonstrate any other degenerative changes radiographically.
The third stage of degeneration is marked by thinning of the articular cartilage. This is also difficult to evaluate initially, but as the cartilage erodes away, it becomes more apparent. At this stage, patients often begin to develop significant clinical symptoms. Facet joints with articular cartilage thinning or subarticular bone erosions frequently are associated with sciatic or low back pain.1 The stimulation of naked nerve endings within the facet joints, at the level of the exiting nerve root, is a common problem.
MR imaging is not the modality of choice for evaluating the facets. CT imaging is far better at demonstrating the changes seen in facet joint degeneration. The fourth stage of degeneration, subarticular bone erosion, is characterized by the reaction of the cortical bone adjacent to the facet joint from its exposure to synovial fluid, causing resorption in the articular processes or the adjacent laminae.
Bone sclerosis frequently is associated with subarticular erosions, as well as synovial cysts in the subchondral bone, caused by synovial fluid being forced into the weakened bone. The final stage of degeneration is hyperostosis, in which the spongy medullary bone is transformed into dense bone and osteophytes form; these degenerative changes are well-demonstrated with CT imaging. Osteophytes that form on the medial surface of the articular processes can cause spinal stenosis, compressing the spinal nerves. Degenerative calcifications of the joint capsule and the ligamentum flavum also can occur.
Synovial cysts are uncommon lesions that develop in degenerating facet joints from the herniation of synovium and synovial fluid through the joint capsule.
This lesion often is associated with intersegmental instability, caused by degenerative joint disease or previous spinal surgery. Generally, the clinical symptoms are low back pain, with or without sciatic pain, usually without positive mechanical signs or electromyographic evidence of root compression. This is a fancy way of saying that classic orthopedic or neurological findings will not confirm the diagnosis.
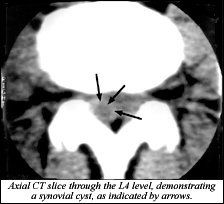
Imaging the affected joint with CT is the easiest way to confirm a diagnosis. An MR scan can demonstrate the cyst if it is large and filled with fluid at the time of the scan. (Note: A useful and related site can be found at www.spine-health.com.)
Reference
- Carrera GG, Haughton VM, Syvertson A, Williams AL. Computed tomography of lumbar facet joints. Radiology 1981;134:145.
Deborah Pate, DC, DACBR
San Diego, California
Click here for more information about Deborah Pate, DC, DACBR.