So, doctor, you think that spinal adjusting will relieve chronic bed-wetting in children? I doubt it, and the few studies published in the scholarly literature in chiropractic, although far from conclusive, are not encouraging (e.g., Gemmel & Jacobson, 1989; Leboeuf et al., 1991).
Recruit or identify from your practice 20 children, ages 5-15, who wet the bed on a regular basis (two or more nights per week) according to parental estimate. After your customarily thorough preliminary examination and history taking to rule out that two percent of children whose chronic enuresis is attributable to infection, anatomic anomaly, frank neurogenic lesion and/or obstruction, and assuming you have decided, by whatever means, that the children are candidates for adjustive care, begin by training mom or dad in a standard method of detecting and recording dry/wet nights. The parent should manually examine the child's bed sheets each morning before the child gets up and should make a dichotomous choice: the bed is wet or dry. "Damp" beds are recorded as wet. The parent should mark a calendar (accessible only to the parent) each morning after the bed sheet inspection to record a dry or wet night. The calendar recordings should be surrendered to you or your office each week to enable you to tabulate the child's progress or lack thereof.
By the way, if the parent and child are willing, you might want to have the child keep a record of dry and wet nights also; that's good psychological therapy, since it keeps the child focused on the target problem, but the record that you, as clinician, will be interested in monitoring is the parents' calendar, since those data are more likely to be accurate.
Your data-organizing task involves grouping consecutive blocks of seven nights (beginning on the first morning) and plotting the number of dry nights out of each consecutive week on a time-series graph (as shown in Figures 1 and 2). You can also plot the parents' pre-baseline estimate of the number of dry nights per week. The baseline then provides a basis for checking whether the child indeed meets the study criteria: Two wet nights/week and for judging the accuracy of parental estimates.

Figure 1: Time-series data plot of an imaginary enuretic child whose parent estimated three dry nights per week at initial clinic visit, indicated by unfilled circle and the legend "E." During the initial, pre-adjustive recording phase (baseline), the child evidenced 4, 2 and 3 dry nights per week. During weeks 4 through 12, the child was administered some form of adjustive intervention, and experienced 2, 1, 3, 4, 2, 1, 3, 1, and 2 dry nights per week. These data suggest no significant change as a function of adjusting.
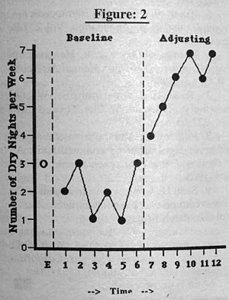
Figure 2: Time-series data plot of an imaginary enuretic child whose parent estimated three dry nights per week at initial clinic visit, indicated by unfilled circle and the legend "E." During the initial, pre-adjustive recording phase (baseline), the child evidenced 2, 3, 1, 2, 1, and 3 dry nights per week. During weeks seven through 12, the child was administered some form of adjustive intervention and experienced 4, 5, 6, 7, 6, and 7 dry nights per week. These data suggest a clinically important arrest of enuresis. Note that the baseline duration in this example is twice as long (6 weeks) as that for Figure 1, and that change (i.e., improvement) is not apparent until adjusting is implemented.
After you've accumulated 20 consecutive cases and plotted all the data on time-series graphs, your next task will be to determine how many of the 20 children experienced 14 consecutive dry nights during the adjusting phase. The 14 consecutive dry night criteria for initial arrest of bed-wetting is somewhat arbitrary, but since it has been employed in a good number of clinical studies of behavioral methods for enuresis (e.g., Azrin et al., 1974, 1979; Azrin & Thienes, 1978; Keating et al., 1983), it provides a somewhat standardized yardstick against which to compare your results. Since summaries of previous clinical trials of various methods of bed-wetting therapy have suggested that 30 percent of children in waiting-list control groups may experience an initial arrest (perhaps a placebo effect or perhaps merely maturation?) you should hope that more than six of your 20 young bed-wetters do as well under your adjustive regimen. By the way, 30 percent initial arrest rates are also about all that can be expected when enuretics receive psychotherapy for their nighttime wetting. The implication here is that although chronic functional enuresis of childhood may cause emotional problems for the child, and may respond to certain behavioral intervention, it doesn't seem to have much of a psychological etiology.
Regardless of whether the results you obtain during adjusting please or displease you, your next obligation is to write up your methods, results, and conclusions for publication in a critically reviewed, scholarly journal. In fact, it is probably more important that you publish your "negative" results than those that seem to support "what we always knew was true," although some doctors may gag on that notion. Make sure to follow the scientific literature in chiropractic while you're conducting your project so that your finished report will be up to date with the work of other chiro-investigators.
Presumably, but not necessarily, you'll wish to submit your completed paper to a quality journal within the chiropractic profession such as the JMPT, Chiropractic Technique, the Chiropractic Journal of Australia, the European Journal of Chiropractic, or the Journal of the Canadian Chiropractic Association. Please don't waste your time by submitting your hard-earned data to trade magazines (i.e., forget the Digest, the ACA Journal, and the ICA Review). If your work is good enough to be shared, its good enough to be charted in a critical, scholarly arena! That's where it counts. Make sure you've followed the "Instructions for Authors" that these journals provide, so as to limit the amount of revising you have to do (and revise you will undoubtedly be required ... that's the name of the game for all research novices).
Here are a few parting thoughts: The projects sketched above shouldn't take more than a year or two, if you work at it steadily. You can expect to be surprised at how many details must be attended to, and at how many "cracks in the floor" you never noticed before (e.g., mom forgot to send the data, the family goes on vacation, the bed-wetter develops the flu). Although it's interesting work, it's also tedious at times -- not for dreamers and wannabes, but for those who will keep their noses to the grindstone.
Moreover, if you take your hypotheses seriously and actually submit them to the rigors of the time-series designs mentioned above, you will not be "proving" anything to the scientific community, but you will have become a part of the scientific community. No matter how your data turn out, you will not be justified in claiming that you have "proved chiropractic works" (yuck!), but you will have taken an important step in helping to improve the quality of chiropractic care by increasing the knowledge base available to other clinicians and investigators. Even if your observations show that children under adjustive care are more likely to wet than before you adjusted them, you will have contributed to fulfilling the "prime directive in chiropractic": to help patients. That's what it is all about -- that's the big idea. Good luck.
References
Azrin NH, Hontos (Thienes) P, Besalel-Arzin V: Elimination of enuresis without a conditioning apparatus: an extension by office instruction of the child and parents. Behavior Therapy, 10(1):14-9, 1979.
Azrin HN, Sneed TJ, Foxx RM: Dry-bed training: rapid elimination of childhood enuresis. Behavior Research & Therapy, 12:147-56, 1974.
Azrin NH, Thienes PM: Rapid elimination of enuresis by intensive learning without a conditioning apparatus. Behavior Therapy, 9:342-54, 1978.
Gemmell HA, Jacobson BH: Chiropractic management of enuresis: time-series descriptive design. Journal of Manipulative & Physiological Therapeutics, 12(5):386-9, October 1989.
Keating JC, Butz RA, Burke E, Heimberg RG. Dry-bed training without a urine alarm: lack of effect of setting and therapist contact with child. Journal of Behavior Therapy & Experimental Psychiatry, 14)2):109-15, 1983.
Leboeuf C, Brown P, Herman A, Leembruggen K, Walton D, Crisp TC: Chiropractic care of children with nocturnal enuresis: a prospective outcome study. Journal of Manipulative & Physiological Therapeutics, 14(2):110-5, February 1991.
Joseph C. Keating Jr., Ph.D.
Los Gatos, California
Editor's Note: The title of Dr. Keating's last article (Oct. 23rd) should have been "Philosophy Doesn't Equal...." We retitled his article to read, "Clinical Experience, Not Philosophy, Produces Competence," which Dr. Keating felt gave the article a slant that did not acurrately reflect his ideas or the theme of his article. Our apoligies to Dr. Keating.
Click here for previous articles by Joseph Keating Jr., PhD.





