In a typical chiropractic practice, most patients are treated for a variety of back and neck complaints. As a result, the general public often pigeonholes chiropractors as "back doctors," which has been our cross to bear for many years.
I remind you of this because extremity issues (feet, shoulders, knees, etc.) are extremely common. Knee pain is pervasive in our patient population, and I know you have at least a few current patients who are coming to you with pain in that region. It might interest you that arthritis or degenerative joint disease picks the medial/inner knee as the second most common area of the body to affect. In fact, arthritis is the most common disease to affect the knees.1
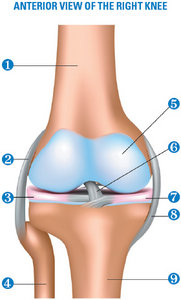 1. Femur
1. Femur
2. Lateral collateral ligament
3. Lateral meniscus
4. Fibula
5. Articular cartilage
6. Anterior cruciate ligament
7. Medial meniscus
8. Medial collateral ligament
9. Tibia
Knee Joint Anatomy
To diagnose a knee problem, the key is a proper examination and clinical history of the patient.2 The knee joint consists of the femur, tibia and the patella. Simply stated, the knee is a hinge joint that allows for flexion / extension and some internal / external rotation. The femur and tibia bones have their movements cushioned by the menisci, which sit on the medial and lateral tibial plateaus.
The ligaments that do the bulk of the work in the knee are the anterior cruciate, posterior cruciate and medial / lateral collateral ligaments. Throw in the quadriceps femoris, adductors, sartorius, ITB, tibialis anterior, gastrocnemius and soleus muscles, and you have all the major players. Entire books have been written on knee function, so I won't attempt to over-dissect this in one article, but I do want to cover functionality and clinical usefulness. The knee can be adversely affected by external and internal trauma, as well as repetitive injuries.
Don't Let the Trauma Fool You
Let's set the stage and get into the mindset of the average knee patient as they present to your office. I want to be clear about one thing that many of us lose sight of: Just because the patient presents to you after an "injury to the knee" does not mean it answers all of your questions about why there may be damage present. Most patients actually come to your office with their knee predisposed to being injured, even in the absence of any trauma.
I am a proponent of foot and arch stability for patients. Knee pain can be a sign of lack of decent support for the medial longitudinal, lateral longitudinal and transverse arches of the feet, creating stress and pain farther up the kinematic chain.
Recall that in healthy gait, the human heel strikes the ground in a slightly inverted and supinated position. The ankle / heel then flatten out and the tibia / femur internally rotate to allow the arches to fall gently toward the floor into normal foot pronation. The arches drop just enough so that foot stability is still maintained and the forces are transferred from the ground to the heel, to the center of the ankle and upward through the center of the knee joint.
 Adjusting the knee: medial femur-tibia
Unfortunately for us humans, genetics, being bipedal and wearing shoes that are often not supportive enough for our feet will create problems. Our foot arches fall more than they should, creating feet that are flatter than they should be. This, in turn, creates more medial stress on the feet, ankles and knees because there is too much internal rotation of the tibia and femur bones.
Adjusting the knee: medial femur-tibia
Unfortunately for us humans, genetics, being bipedal and wearing shoes that are often not supportive enough for our feet will create problems. Our foot arches fall more than they should, creating feet that are flatter than they should be. This, in turn, creates more medial stress on the feet, ankles and knees because there is too much internal rotation of the tibia and femur bones.
If one has flat arches, this drops the foot and puts stress on the inner foot / ankle. The increased medial rotation of the tibia and femur shifts the patella medially as well. This puts rotational stress and tension on the ACL, medial meniscus and medial collateral ligament, eventually creating pain. Since overpronation or excessive pronation of the feet affects a large portion of our population these days, it is understandable why medial knee pain is so prevalent.
Common Knee Presentations
Do any of these common knee presentation characteristics fit any of your current knee cases?
- Developed knee pain over time: The pain was quite tolerable in the initial stages and the patient can usually work or stretch through it. But lately, it has become worse and worse, and even stays around after they finish with their activities. Generally, the onset is insidious. In fact, the patient is very upset and confused as to why they have pain in the first place. It's also interesting because allopathic physicians and the other practitioners often cannot explain why the pain exists. Sometimes there is a description of a changing activity level (training harder, covering more miles, etc.).
- Pain commonly located in the medial / anterior region of the knee. It can be described at times as being located under the patellae or radiating from the front to the inner to posterior knee as well.
- Knee pain aggravated by weight-bearing stress or performing their sport. Some will get to the point that they have to physically stop what they are doing and sit down to rest. Then they can get back up and continue on for a little longer.
- Traumatic-onset or "single incident" traumas obviously give the patient pain and damage to specific knee areas. Usually, we see a lot of ACL tears, medial meniscal degeneration and medial collateral ligament damage.
- Knee pain that persists despite physiotherapy modalities, exercises, rehabilitation, massage, etc. This is most often true in cases of non-traumatic or insidious onset, in which tissues were gradually affected, which results in the above treatments failing to produce significant changes or lasting effects. In single-incident traumas, rehab can be more successful.
 Adjusting the knee: medial tibia-femur
Examining the Patient
Adjusting the knee: medial tibia-femur
Examining the Patient
Since you have already spoken to the patient and taken their history, you have a good idea of which structures are involved. Is it possible that ligaments and/or muscles could be torn? Use your orthopedic testing to find out. Most of the time, the patient will complain of insidious onset of pain, so structures are intact, but very stressed or irritated. Even a mild tear can heal if the knee is realigned properly. Many patients with moderate to severe foot overpronation can be one movement away from a devastating knee injury or painful episode.
Your palpation is very powerful here because while the patient is supine or sitting with their knee supported by a pillow underneath, you can do passive range of motion (PROM) and palpation, and figure out how the structures feel.
Chiropractic Adjustments
In most cases of knee pain, the bones have misaligned according to the excessive foot pronation patterns we identified earlier: medial tibia, medial femur and medial / inferior patella. For these three adjustments, the patient should be sitting or supine with a pillow under their knee to prevent full extension or knee locking. The doctor stands to the side of the involved leg with the inferior hand grasping the proximal tibia and the superior hand grasping the distal thigh.
 Adjusting the knee: medial-inferior patella
All you have to do is to pre-stress the bones from medial to lateral about the long axis of the bones. Then your thrust is a very gentle continuation of the pre-stress. Don't expect loud audibles on these adjustments.
Adjusting the knee: medial-inferior patella
All you have to do is to pre-stress the bones from medial to lateral about the long axis of the bones. Then your thrust is a very gentle continuation of the pre-stress. Don't expect loud audibles on these adjustments.
What about adjustments in the prone position? Of course you can do these. Remember that the femur and tibia bones are long bones and you need to see how they have misaligned in a three-dimensional way. When a patient is prone, the medial rotation of the femur and tibia bones will feel like the medial tibial plateau and the distal, medial femur are sticking out at you. You can use your hand-held adjusting instrument to maneuver or de-rotate the medial aspects of these bones. It is almost like you are spinning the bones back from medial to lateral.
Other Care Strategies
Finally, you can discuss scanning your patients for three-arch, custom, flexible orthotics. This will help to support the feet, ankles and knees, all the way up to the neck. You can also discuss knee braces or elastic sports taping if you feel it is appropriate. Stretching, strengthening and rehabilitation exercises of your choice will also help.
In some cases, it's the body parts that aren't hurting which help you understand the ones that are. The feet are a prime cause of problems that manifest throughout the body. If your patient has knee problems, make sure you check those feet. Having no pain does not mean they are fine!
References
- Knee Problems: Questions and Answers About Knee Problems. National Institute of Arthritis and Musculoskeletal and Skin Diseases.
- Monk D. "Examining the Knee Joint." Emerg Nurse, 2013 Apr;21(1):28-36.
Dr. Kevin Wong, earned a BS in exercise physiology from the University of California – Davis and his DC degree from Palmer Chiropractic College West. He practices in Orinda, Calif., and serves the Lamorinda, Berkeley, Walnut Creek and many other East San Francisco Bay Area communities. He is an expert on foot analysis, walking and standing postures, and orthotics, and lectures nationwide on spinal and extremity adjusting.




