"Acute low back pain" is the number one patient complaint that leads to chiropractic visits. Our treatment should have as its goal the maintenance or resumption of normal functional activities. Chiropractic appropriately emphasizes the role of manipulation in reducing activity intolerances. Other "tools of the trade" include improved psychosocial attitudes or coping skills, and stabilization training through activity modification advice or exercise.
Goals for this Series - to Learn:
- what the "tools of the trade" are for a DC utilizing active care;
- how the stability model is revolutionizing rehab; and
- the role of psychosocial factors in treatment outcome.
Why don't chiropractors use active care more? Some common attitudes include comments like:
- "Most patients respond to what we are already doing, so why change anything?"
- "Patients won't comply with self-treatment, so why should we prescribe it?"
- "Doesn't exercise prescription require great expenses for equipment, space, expertise and time?"
Each of these concerns will be addressed in this series. This article elaborates on:
- the natural history of low back problems;
- barriers to recovery;
- the place of active care; and
- the primary muscles responsible for low back stability.
Evidence-Based Healthcare (EBH)
There is a new paradigm in health care practice, a radical shift away from knowledge based on authority and clinical experience focusing on the rules of evidence. This is designed for evaluating the huge volume of medical literature and disseminating the most valid and important findings to practitioners. It utilizes a hierarchy of methodologies best suited for clinically testing the efficacy of drugs. Large randomized clinical trials (RCTs) get the highest value; expert opinion gets the lowest value.
Limitations of Guidelines
There is very little in the guidelines about how to improve patients' activity tolerance! They are based exclusively on evidence (even if scant) and not on expert clinician opinion. There is no evidence that they improve the quality or reduce the cost of care. The problem in physical medicine is not a large volume, but rather a scarcity of high-quality evidence. Tonelli argued that expert opinion could be regarded as the "best, not poorest methodology."1
According to Sackett, "clinical expertise should be informed - but not replaced by evidence."2 Recently, Rossignol, et al., concluded that "education must be part of a new system of care which is easy for the doctor."3 More thorough explanations to patients and their participation in decision-making were found to be more valuable. The "take-home" message is that guidelines are necessary, but are not going to improve quality because they are just not sufficient.
Natural History of Back Problems, and Which Factors Influence It
Based on large-scale data on low back disability, most sufferers recover within six weeks. There is a high recurrence rate, and five percent have chronic pain, but the majority of chronics are not disabled. Therefore, the goal of care is to maintain physical functioning.4
What are "meaningful" outcomes? According to Deyo, a few domains should be monitored quantitatively for progress. They are pain (duration, intensity, radiation), function (activity intolerances , physical performance capacity), and disability/return to work status, psychosocial status. 5 A number of factors that are demonstrated to impact recovery have been identified. Some of the most important ones have been called "yellow flags." In contrast to "red flags'" of serious disease which require urgent attention, "yellow flags" should be identified and addressed, but the consequences for missing them is not so severe.
There are various "yellow flags" which alert us to a potential poor recovery. Identifying these early in care allows for improved prognostication and selection of management approach that matches the needs of the patient.
"Yellow Flags": Psychosocial Predictors of a Poor Outcome18
- anxiety;
- locus of control;
- depression;
- job dissatisfaction; and
- fear avoidance beliefs.
Are there treatments that are documented to be superior to "tincture of time"? Aren't adjustments the "gold standard" for treating patients? Are there other treatments that are also "evidence-based" for back problems? What follows is a summary of some of the more important evidence that active care is superior to "tincture of time" or other modalities at different phases of the recovery process. By "active care," what is meant is anything from basic advice to "stay active" to supervised machine-based exercise routines.
Acute Patients - Advice to Stay Active
Information and advice emphasizing the value of fitness and safety of resuming activities achieved superior outcomes to advice which reinforced rest, activity restrictions and the notion that the spine was injured or damaged (arthritis, herniated disc).6
Acute Patients - Exercise
Fordyce found that early behavior modification through exercise reduced disability 1 year later.7 Linton's studies saw an eightfold reduction in the risk of becoming chronic from information designed to reduce fear and anxiety and provide self-care advice.8 Reassuring workers and encouraging resumption of ordinary activities was superior to medication, bed rest or mobilization exercises, concluded Malmivaara.9
Subacute Patients - Exercise
A study by Lindstrom in 1992 concluded that a graded activity program reduced disability more than traditional care.10
Chronic Patients - Exercise
Indahl's 1995 study resulted in the following: "Education designed to reduce fear. Patients informed that light activity would not injure the disc, but instead speed recovery. Return to work rate was double control group."11 In addition, Sullivan noted specific spine stabilization exercises achieved more superior outcomes than isotonic exercises in chronic patients with spondylolysthesis.12
Other studies include: "Isotonic regime emphasizing endurance training successful in improving outcomes;"13 "Exercise was shown to be superior to passive care in treating failed back surgery patients. Low-tech exercise (McKenzie and Stabilization) superior to high-tech exercise (istonics and Cybex)."14
Common Denominators of Successful Care for Chronic Patients
- thorough physical and functional examination performed;
- report of findings given;
- emphasis on self-care;
- reduction of any unfounded fear or anxiety about pain;
- crystal clear recommendations about activities/exercise; and
- avoidance of excessive "high tech" testing or bed rest prescription.
Implementing Change: How to Add Active Care to Your Practice
We now know why active care is important, but we need to understand how to integrate it with passive care. What new evidence can be used to improve the quality of our practices? Psychosocial factors are essential for prevention of acute pain becoming chronic while biomechanical factors relating to joint stability are revolutionizing the place of manipulation and exercise.
The psychology of back pain is very important, especially for prevention and treatment of the chronic problem. Active care should begin on day one, with advice about activity modifications and self-treatment (e.g., McKenzie). "Our message should be designed to avoid reinforcing the 'sick' role," wrote Waddell in 1998.15 That psychological factors relate to the recovery of a patient does not minimize the importance of neurophysiological or biomechanical aspects of the back pain problem. The question of the role of stability in the mechanism of injury of low backs is crucial. Only by understanding stability can we see how trivial load can cause painful injury.16
What is the role of manipulation in promoting stability? What is the role of exercise in promoting stability? These questions are essential to understand in order to be successful integrating exercise into chiropractic practice. The functional reactivation/restoration approach is best summarized by McGill: "Evidence from tissue-specific injury generally supports the notion of a neutral spine (neutral lordosis) when performing loading tasks to minimize the risk of low back injury."17
Manipulation is suited for reducing pain and promoting mobility. In contrast, exercise is designed to reduce fear-avoidance behavior and promote stability. Stability requires a 360-degree approach. The goal is to train postural control (i.e., position sense) of the back's "neutral position," and then to train endurance of the muscles that can maintain "neutral" in all 360 degrees (anteriorly, laterally, and posteriorly).
What are the stabilizers of the spine? Posteriorly - the trunk extensors; anteriorly - the trunk flexors; and laterally - the quadratus lumborum. All of these muscles should be re-educated to provide stability during functional tasks. This requires awareness of how to activate them, and then the isolation of them during low-load endurance training while neutral spine postures are maintained in functional activities.
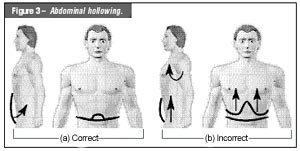
Exercises can begin with the following "big three:" quadruped one-leg raise, side support on knees, and abdominal hollowing (see Figures 1,2,3 ).
The modern approach focuses on function, not just relief of symptoms. In the report of findings it is important to establish the following goals of care: to reduce pain, restore function and keep the patient independent. This requires a strategic program heeding "best practice" approaches of manipulation, active care, outcomes management and a biopsychosocial approach (see below).
"Best Practice" Model (the benchmark!)
- diagnostic triage: rule out "red flags," and provide reassurance;
- pain relief approaches - manipulation, medication, modalities, McKenzie method;
- functional reactivation;
- level one active care advice to gradually resume normal activities;
- level two active care exercise to retrain "weak link";
- biobehavorial approach;
- nonresponders with "yellow flags"; and
- outcomes management, appropriate documentation.
The reflective practice-based model presented here can be facilitated by self-audit of your practice procedures. Chart review should reflect that the diagnostic has been performed; "yellow flags" have been assessed (thorough questionnaire); manipulation has been offered; the patient has been advised to stay active; self-treatment has been recommended and instructed (active care); referral was made if "red flags" of serious pathology, cauda equina, or unresolving neurological condition were present; and additional investigations or treatment were arranged if back pain was nonresponsive within six weeks.
EBH can be applied to your practice through a reflective, practice-based learning model. This is a new paradigm of care and learning which utilizes a problem-solving approach to learn. Your practice is the central place of learning rather than a classroom. It is truly active learning rather than a passive, didactic approach. "Monday morning" application is the key! EBH is grounded in critical thinking and evaluation of the "best evidence."
The next three articles in this series will cover the biopsychosocial model, the stabilization system and the kinetic chain and present the "tools of the trade" for utilization in your practice. The goal is to facilitate a shift of your practice to a new model. Integration of EBH occurs at your own pace. I hope it motivates you to "life-long" learning.
References
- Tonelli MR. In defence of expert opinion. Academic Medicine 1999:74(11);1187-92.
- Sackett DL, Rosenberg WMC, Muir Gray JA, Haynes BA, Richardson W. Evidence based medicine: What it is and what it isn't. British Medical Journal 1996: 312;71-72.
- Rossignol M. Coordination of Primary Health Care for Back Pain. Spine 2000:25; 251-259.
- Carey TS, Mills Garret J, Jackman AM. Beyond the good prognosis. Spine 2000:25;115-120.
- Deyo RA. Low back pain. A primary care challenge. Spine 1996:21;2826-2832.
- Burton K, Waddell G. Information and advice to patients w/ back pain can have a positive effect. Spine 1999:24;2484-2491.
- Fordyce WE, Brochway JA, Bergman JA, et al: Acute back pain; a control-group comparison of behavioral vs. traditional management methods. J Behav Med 1986:9;127-140.
- Linton SJ, Hellsing AL, Andersson D. A controlled study of the effects of an early intervention on acute musculoskeletal pain problems. Pain 1993:54;353-359.
- Malmivaara A, Hakkinen U, Aro T, et al. The treatment of acute low back pain - bed rest, exercises, or ordinary activity? N Engl J Med 1995:332;351-5.
- Lindstrom A, Ohlund C, Eek C, et al. Activation of subacute low back patients. Physical Therapy 1992:4;279-293.
- Indahl A, Velund L, Eikeraas O. Good prognosis for low back pain when left untampered: A randomized clinical trial. Spine 1995:20;473-7.
- O'Sullivan P, Twomey L, Allison G. Evaluation of specific stabilizing spondylolysis or spondylolysthesis. Spine 1997:24;2959-2967.
- Manniche C, Lundberg E, et al. Intensive dynamic back exercises for chronic low back pain. Pain 1991:47;53-63.
- Timm KE 1994. A randomized-control study of active and passive treatments for chronic low back pain following L5 laminectomy. JOSPT 20:276-286.
- Waddell G. The Back Pain Revolution. 1998 Churchill Livingstone, Edinburgh.
- McGill S. Stability: from biomechanical concept to chiropractic practice. J Can Chiro Assoc 1999:43;75-87.
- McGill SM. Low back exercises: Prescription for the healthy back and when recovering from injury. In: Resource Manual for Guidelines for Exercise Testing and Prescription 3rd Edition. Williams and Wilkins, 1998.
- Kendall NAS, Linton SJ, Main CJ. Guide to assessing psychosocial yellow flags in acute low back pain: Risk factors for long-term disability and work loss. Accident Rehabilitation and Compensation Insurance Corporation of New Zealand and the National Health Committee. 1997, Wellington, NZ. Available from http://www.nhc.govt.nz.
Craig Liebenson,DC
Los Angeles, California
Click here for previous articles by Craig Liebenson, DC.