When we think of lower back pain, we tend to think in terms of the lower lumbar spine and the SI joint. These joints and their discs are obviously important. However, we tend to miss fixations that occur just above – in the upper lumbar spine.
One important aspect of the upper lumbar spine is the sensory nerve supply that begins there. I have talked about this in relation to the thoracolumbar junction (T-L junction).1 In this article, let's focus on the upper lumbar part of the T-L at L1-2-3.
Robert Maigne2 writes that in his dissections, he noted a tender nodule along the course of the peripheral sensory nerves, 7-8 cm lateral to the midline, just below the iliac crest. He stated that it usually originated from L1, but could be from L2 or L3 as well. This is the superior cluneal nerve, a peripheral sensory nerve that supplies sensation to the skin over the flank or quadratus lumborum area, as well as over the gluteal area.
We tend to think in terms of pain coming from a muscle, if bodywork is our background; or from the spine, as chiropractors. This model invites us to remember that pain can come from irritated peripheral sensory nerves. The location of this particular pain is distal enough that we tend to think of the pain as L4-5, L5-S1, or as SI-generated pain. It could be, but often low back or pelvic pain is coming from higher in the spine; from either the lower thoracics or the upper lumbar, at the origins of the superior cluneal nerve.
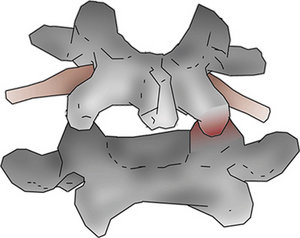 Fig. 1: The picture shows an upper vertebra, unable to flex open on the right side. Note the redness, indicating irritation of the facet that cannot open. Note the positioning of the upper vertebra, stuck in extension, right rotation and right sidebending. The vertebra resists flexion, left rotation and left side-bending.
Patient Presentation
Fig. 1: The picture shows an upper vertebra, unable to flex open on the right side. Note the redness, indicating irritation of the facet that cannot open. Note the positioning of the upper vertebra, stuck in extension, right rotation and right sidebending. The vertebra resists flexion, left rotation and left side-bending.
Patient Presentation
How do these patients present? First of all, they may or may not complain of pain in the area we suspect is its origin, the upper lumbar spine. Or they may be vague; many patients seem to have a hard time localizing their pain. They complain that their low back or buttock area hurts. When asked to be more specific, they may describe the lower lumbar area or they may complain of flank pain. If they complain of sciatica or buttock pain, the pain is unlikely to go below the knee.
If you trace the nerves, you will usually find tenderness and/or mild edema along the course of the superior cluneal nerves. Start at the irritated spinal segment and follow an oblique path, through the buttock and down into the posterior hip area.
One of your primary indicators for this phenomenon is going to be the tender points found just below the iliac crest, and the response of these tender points to your upper lumbar manipulation. If you are on the right track, when you free up the stuck upper lumbar segments, the distal tenderness diminishes.
Assessment Tips
One way to start your assessment of both the upper lumbar and the lower thoracic spine is to palpate the nodules just below the iliac crest. These are along the lines of the peripheral sensory nerves and present as distinct, palpable, tender lumps, just below the iliac crest. The more medial tender point, 7-8 cm lateral to the midline, is along the superior cluneal nerve and points you to L1-L3.
 Fig. 2: Positioning for palpating the lumbar spine to detect segments resisting flexion. Use your left hand on top of the patient's left shoulder to move them into lumbar flexion, left side-bending and left rotation. Feel for which segments don't move.
The more lateral tender points, probably best described as being along the T10-11-12 peripheral sensory nerve (although some may refer to it as another branch of the superior cluneal nerve), 10-12 cms lateral to the midline, point you to the T10-11-12 spinal fixations. The concept of a more lateral tender point connected to the upper part of the T-L is from John Lyftogh, MD, or neuroprolotherapy.3 When you find these tender points, you almost always find fixations on the homolateral side of the spine.
Fig. 2: Positioning for palpating the lumbar spine to detect segments resisting flexion. Use your left hand on top of the patient's left shoulder to move them into lumbar flexion, left side-bending and left rotation. Feel for which segments don't move.
The more lateral tender points, probably best described as being along the T10-11-12 peripheral sensory nerve (although some may refer to it as another branch of the superior cluneal nerve), 10-12 cms lateral to the midline, point you to the T10-11-12 spinal fixations. The concept of a more lateral tender point connected to the upper part of the T-L is from John Lyftogh, MD, or neuroprolotherapy.3 When you find these tender points, you almost always find fixations on the homolateral side of the spine.
I first wrote about this concept three years ago. It has stood the test of time in my practice, and applying these principles continues to help solve lower back and gluteal pain that might otherwise not respond. The T-L junction is a transition zone, where the lumbar lordosis begins to convert to the thoracic kyphosis. This is a stress zone; a site where faulty movement often occurs.
Why do we miss this? As I mentioned above, we think more often of the lower lumbars and SI. I am grateful to Mike Boyle, who introduced me to the joint-by-joint model. The lower lumbars tend toward instability; the upper lumbars and lower thoracics tend toward stiffness and a lack of mobility. If our tool is manipulation, aiming at stiff areas is more useful; at least most of the time.
My spinal assessment techniques draw from a mix of chiropractic motion palpation, osteopathic muscle energy and assessment for tenderness. Muscle energy first focuses on whether the segment is flexed or extended. I tend to interpret this through my motion palpation training: What is fixated? Does the segment resist flexion or extension? Once you have determined this, you can fine tune for resistance to lateral bending and/or rotation.
In the lower thoracic, the stuck segments most commonly resist extension. In the upper lumbar, near the apex of the lumbar lordosis, the segments commonly resist flexion. (It took me a long time to figure this out. I think it is another piece of the spinal puzzle I had been missing for a long time.)
It is easy to miss the lumbar segments that resist flexion. My initial training was to palpate from behind, with a scanning posterior-to-anterior pressure, to find stuck areas and then try to isolate to the offending segment. If you screen this way, you will miss the segments that resist flexion as they move in a near-normal way into extension.
If you are palpating in the paraspinal area, assessing which side resists rotation, you are applying pressure from behind. This fixation is even more difficult to find if you palpate with the patient prone, as the lumbar spine relaxes into extension. It is easy to miss the segments that primarily lack flexion.
You have to get inferior to the segment and lift it upward to find these restrictions. You can do this with your flexion-distraction table. You can also do it sitting by having the patient slump forward and then lifting the segment from below with your thenar pad or thumb. You can push the spinal segments into flexion in the midline, and you can push superior on the mammillary processes, getting a sense of which side of the facet is stuck closed.
Muscle energy technique has an elegant palpation for this area. Place your thumbs parallel to each other, over the segment in question. Have the patient slump forward into flexion. If one side is stuck in extension and resists flexion, the vertebral body will rotate to that side. You will notice your thumb on that side coming back toward you. Watch your thumbs reposition as the vertebra rotates. It is more visual than classic chiropractic motion palpation. This listing is called an ERS in muscle energy terminology, as the vertebra is extended, rotated and side-bent to the homolateral side.4
Another indicator of lack of flexion versus lack of extension is tenderness. If you gently extend the patient while you push on the mammillary process, do you elicit tenderness? If you get below and flex the patient as you push on the mammillary process, does that elicit tenderness? The motion that is restricted will increases the tenderness over the facet or mammillary process.
Editor's note: Part 2 of this article appears in the Nov. 1 issue and discusses spinal correction techniques for upper lumbar fixations.
References
- Heller M. "Thoracolumbar Junction or Superior Cluneal Nerve Entrapment Syndrome: A Hidden Source of Low Back & Pelvic Pain." Dynamic Chiropractic, Nov. 4, 2011.
- Maigne JY, Maigne R. Trigger point of the posterior iliac crest; painful ilio-lumbar ligament insertion or cutaneous dorsal ramus pain? Arch Phys Med Rehab, 1991;72;734-7.
- Lyftogt J, from video presentation, Hawaii Neural Prolotherapy Workshop, November 2011.
- Heller M. "Palpation of the Upper Lumbar Spine" (YouTube video).
Click here for more information about Marc Heller, DC.





