Contributed by Claire Johnson, DC, MsEd, PhD, Bart Green, DC, MsEd, PhD, DC, MPH, PhD (cand.), and Michael Haneline, DC, MPH
The Zika outbreak continues to spread across the continental United States and U.S. territories. We offer this brief overview on this important public health problem for the practicing doctor of chiropractic.
Zika virus is a Flavivirus similar to West Nile virus and yellow fever. Although the Zika virus was first identified in Africa in 1947, it was in April 2015 that an outbreak began in Brazil, resulting in the recent pandemic.1 The virus is primarily spread by infected mosquitoes (e.g., Aedes aegypti and Aedes albopictus), but can also be spread through sexual activity, blood transfusions and from mother to fetus.1
2. What Are the Signs and Symptoms of Zika?
People who are infected have few, if any, signs or symptoms of infection. When present, symptoms are typically mild and last a few days to a week. Infected people may experience back pain, muscle pain and headaches.1 In extreme cases, damage to the nervous system can result in permanent muscle weakness, paralysis and sometimes death.2-3 Signs include fever, rash (see photo) and conjunctivitis.
Pregnant women may not show signs or symptoms, but may still be infected and transmit the infection to the baby in utero.
3. Why Is Zika a Problem?
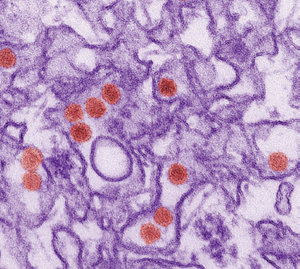 Zika virus (CDC open-access photo: http://phil.cdc.gov/phil/home.asp).
If a pregnant woman is infected with Zika during pregnancy, the baby may have severe nervous system damage or brain malformations, such as microcephaly.4 It is estimated that a third of children born from infected mothers will have severe nervous system deformities and a greater proportion are suspected to have nervous system complications throughout their life.5
Zika virus (CDC open-access photo: http://phil.cdc.gov/phil/home.asp).
If a pregnant woman is infected with Zika during pregnancy, the baby may have severe nervous system damage or brain malformations, such as microcephaly.4 It is estimated that a third of children born from infected mothers will have severe nervous system deformities and a greater proportion are suspected to have nervous system complications throughout their life.5
Adults or children infected with the Zika virus may develop Guillain-Barré syndrome, a progressive nervous system disease wherein the immune system attacks nerve cells, potentially resulting in paralysis and death.
4. What Can Be Done If a Patient Already Has Zika Infection?
Currently, there is no treatment for Zika infection, although many of the symptoms can be managed with palliative care. Doctors of chiropractic may encourage Zika-positive patients to control Zika symptoms by getting rest, staying hydrated, and avoiding nonsteroidal anti-inflammatory drugs (NSAIDS) such as aspirin, because dengue – which is a similar infection – should not be treated with these medications due to bleeding risk.1
Additionally, these patients should take special care to avoid spreading the virus to others. This can be done by controlling mosquito bites and by using barriers, including condoms, for all forms of sex until at least eight weeks after illness for women and six months after illness for men, as the virus appears to last longer in semen than in urine, vaginal fluids and blood. Preventing spread of the virus to others is essential if someone is infected.
5. What Should We Recommend to Patients?
The number of people diagnosed with Zika infection in the U.S. continues to grow. Because there are currently no treatments or vaccinations for Zika, prevention is best.6 All patients can be counseled to do the following to reduce their risk of transmission:
- Prevent mosquito bites (e.g., repellent, clothing, window screens)
- Reduce mosquito breeding sites (e.g., remove all standing water)
- Reduce exposure to mosquitos (e.g., netting, mosquito traps in yard)
- Avoid travel to areas with high levels of confirmed Zika transmission
- Practice sexual safety (e.g., not having sex in areas with Zika virus or with travelers through or from these areas, and using barriers for all forms of intercourse)
 Zika rash on back (CDC open-access photo: http://phil.cdc.gov/phil/home.asp).
In addition, patients considering pregnancy may decide to delay pregnancy depending on potential exposure risk, or change environment or travel plans to Zika-infected regions to prevent exposure.
Zika rash on back (CDC open-access photo: http://phil.cdc.gov/phil/home.asp).
In addition, patients considering pregnancy may decide to delay pregnancy depending on potential exposure risk, or change environment or travel plans to Zika-infected regions to prevent exposure.
6. What Can Doctors of Chiropractic Do?
Doctors of chiropractic should ask all pregnant patients about their travel histories. If you suspect a patient may have Zika, or a pregnant woman may have been exposed through a mosquito bite or sex with a partner who may have been exposed, a blood or urine test should be ordered.7 Contact your state or local health department for information about appropriate testing.
Doctors of chiropractic can work with other health care providers and the Centers for Disease Control and Prevention (CDC) to help educate patients about preventing Zika infection. Zika is a nationally notifiable condition, so a chiropractor who detects a case of Zika must report it – contact local health authorities for procedures.
We must be aware of the risks associated with patients contracting Zika, and the symptoms and signs.8 Zika has been reported across the Continental United States and a visit to the CDC map site shows how many cases are reported in each state.
More Info for Patients
- Zika information for patients: www.cdc.gov/zika/pdfs/fs-zika-basics.pdf
- World Health Organization information on Zika: www.who.int/topics/zika/en/
More Info for All Health Care Providers
- CDC Zika updates: www.cdc.gov/zika/
- Map of Zika outbreak: www.cdc.gov/zika/intheus/maps-zika-us.html
- For providers: www.cdc.gov/zika/pdfs/key-zika-considerations.pdf
- Information about Zika and pregnancy: www.cdc.gov/zika/hc-providers/pregnant-woman.html
When doctors of chiropractic work with local public health officials to share prevention information, we improve the health of our local communities. Through our public health efforts, the chiropractic profession can be a part of the solution for Zika and other public health issues.
References
- Sampathkumar P, Sanchez JL. Zika virus in the Americas: a review for clinicians. Mayo Clin Proc, 2016 Apr;91(4):514-21.
- Cao-Lormeau VM, Blake A, Mons S, et al. Guillain-Barré Syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet, 2016 Apr 9;387(10027):1531-9.
- Dos Santos T, Rodriguez A, Almiron M, et al. Zika virus and the Guillain-Barré Syndrome - case series from seven countries. (Correspondence) N Engl J Med, 2016 Aug 31.
- Mlakar J, Korva M1, Tul N, et al. Zika virus associated with microcephaly. N Engl J Med, 2016 Mar 10;374(10):951-8.
- Lyon J. Zika: worse than thalidomide? JAMA, 2016 Sep;316(12):1246-1248.
- Fauci AS, Morens DM. Zika virus in the Americas - yet another arbovirus threat. N Engl J Med, 2016 Feb 18;374(7):601-4.
- Hennessey M, Fischer M, Staples JE. "Zika Virus Spreads to New Areas - Region of the Americas, May 2015-January 2016." MMWR Morb Mortal Wkly Rep, 2016 Jan 29;65(3):55-8.
- Shuaib W, Stanazai H, Abazid AG, Mattar AA. Re-emergence of Zika virus: a review on pathogenesis, clinical manifestations, diagnosis, treatment, and prevention. Am J Med, 2016 Aug;129(8):879.e7-879.
Click here for more information about Public Health, Wellness & Prevention Contributors.





