My earlier articles on axial discogenic pain focused on assessing midline tenderness, found by palpating with an anterior superior pressure in the interspinous space (see www.chiroweb.com/archives/21/18/08.html).
Axial discogenic pain patients have equivocal degenerative findings or bulged discs on MRI, and have pain with stillness such as prolonged standing or sitting, but do not usually have true sciatica. They usually have difficulty with more vigorous exercise, such as running or other pounding activities. They can also irritate their backs with a simple unguarded forward bend. On a discogram, these patients would show concordant pain responses with higher pressures. These patients are difficult to diagnose, as the pain can easily be blamed on SI or other lumbar joint dysfunction, arthritis, or other factors. I personally have this type of torn disc, so I know the pattern.
There is very minimal peer-reviewed literature on this midline tenderness phenomenon, other than a series of articles from Finland in the late 1990s.1,2 I e-mailed Vaharanta,3 who was kind enough to get back to me. He noted that the testing protocol they used involved a percussive force over the spinous processes, not digital pressure or vibration over the interspinous space.
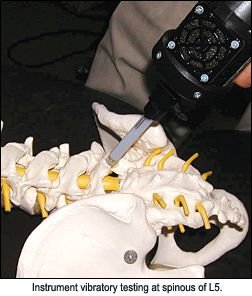
 I recently realized that I had the perfect adjusting tool to do this type of testing. Any similar adjusting tool should work - something that has a relatively hard and small tip, and that can percuss with frequency. Place the tip of the instrument over a lower spinous process, and tap in a posterior-to-anterior direction. Does this elicit pain? I do not know if a tap with a reflex hammer or Activator would produce the same effect. I am now using both digital pressure in a anterior-superior direction between the lower spinous processes, and tapping with my adjusting tool over the lower spinous processes. The digital interspinous pressure will find many tender interspinous spaces. Others will only be tender to the instrument-assisted percussion.
I recently realized that I had the perfect adjusting tool to do this type of testing. Any similar adjusting tool should work - something that has a relatively hard and small tip, and that can percuss with frequency. Place the tip of the instrument over a lower spinous process, and tap in a posterior-to-anterior direction. Does this elicit pain? I do not know if a tap with a reflex hammer or Activator would produce the same effect. I am now using both digital pressure in a anterior-superior direction between the lower spinous processes, and tapping with my adjusting tool over the lower spinous processes. The digital interspinous pressure will find many tender interspinous spaces. Others will only be tender to the instrument-assisted percussion.
Unfortunately, once you have the suspicion of a torn disc, it's difficult to confirm with anything less than the invasive and expensive discogram. There is no gold standard of treatment for this condition. A broad chiropractic approach, including quality stabilization training, midline distraction/decompression, normalizing pelvic and lumbar motion, and optimizing soft tissue dysfunction, can help. Low-level laser or other modalities may be helpful in selected cases. Botanical anti-inflammatories or enzymes can be effective, and magnesium can help with chronic muscle tightness. Decompression machines are currently being promoted. I am not sure if this is a genuine advance in technology or just another expensive fad. You are unlikely to cure these patients, but you can often help them become more functional and stabilize them.
 The medical approach could include epidurals or anti-inflammatory meds. The surgical approach could include lumbar fusion, but I'm sure you know the relatively poor consistency of results from fusion. Artificial disc replacement is another newer surgical tool, which is promising, but the long-term results are still unknown. More recent, minimally invasive approaches usually performed by pain specialists/anesthesiologists include IDET (intradiscal electrothermal), a needle procedure heating the annulus, nucleoplasty, a similar procedure heating the nucleus rather than the annulus, and intradiscal injections, using glucosamine and other growth factors to enhance disc healing. Results are variable for all of these procedures. If the patient has genuinely tried all of the more conservative procedures and still has consistent pain levels above a 5 or 6 out of 10, these procedures may be worth considering. The difficulty with any of these invasive and permanent procedures is that the surgeon/anesthesiologist may be promoting his or her favorite procedure, rather than considering what is best for the patient.
The medical approach could include epidurals or anti-inflammatory meds. The surgical approach could include lumbar fusion, but I'm sure you know the relatively poor consistency of results from fusion. Artificial disc replacement is another newer surgical tool, which is promising, but the long-term results are still unknown. More recent, minimally invasive approaches usually performed by pain specialists/anesthesiologists include IDET (intradiscal electrothermal), a needle procedure heating the annulus, nucleoplasty, a similar procedure heating the nucleus rather than the annulus, and intradiscal injections, using glucosamine and other growth factors to enhance disc healing. Results are variable for all of these procedures. If the patient has genuinely tried all of the more conservative procedures and still has consistent pain levels above a 5 or 6 out of 10, these procedures may be worth considering. The difficulty with any of these invasive and permanent procedures is that the surgeon/anesthesiologist may be promoting his or her favorite procedure, rather than considering what is best for the patient.
I will briefly share my personal experience: I had an IDET in 2000 for my L4 torn disc. The recovery was difficult, but the procedure was somewhat helpful. A chiropractic colleague who had damaged his discs in a snow sledding accident had an IDET with a well-respected doctor, and ended up with ongoing, unrelenting sciatica. He unfortunately had nerves that were somehow burned in the procedure, probably from an anomaly in his anatomy. I suspect that events like this are under-reported in the literature.
I also had a single disc injection of glucosamine and other growth factors into both my L4 and L5 discs in 2005, after another discogram. I am not sure whether this one helped. I did not have rapid or immediate changes, but again, I have the high pressure biomechanical type of disc, where inflammation is not the major factor.
I added another therapy in April 2005. I started doing stabilization exercises, based on basic core principles, Pilates and anusara yoga.4 I realized, one month before my disc injection procedure, that my core really was not as strong as it should be. I committed to doing a consistent 20-minute daily routine. I was already active and fit, but core strength, especially for someone with chronic lower back pain, requires more than ordinary fitness. I have also been extraordinarily aware of my posture at work, at home, and in my ADLs.
I am stronger, I am more resilient, and I have less pain. I handle airplane flights and long drives much better, although these still stress my back. I don't feel like I "go out" easily or am half as "glitchy" in my lower back. The injection procedure may get some of the credit, but I suspect that most of the change was due to the exercise. This is not a miracle cure, but a healing process. I still cannot stand with ease, I still slouch when I sit to decompress my spine, and I still feel better when I wear a lightweight lumbar brace.
I know many of our patients want a quick fix, a magic bullet: "Please fix me, Doc." For those willing to commit the time and energy, to really learn to change their own back mechanics, there is a definite benefit. A good spinal stabilization program is necessary for any chronic back pain. Chronic pain causes inhibition to the stabilizing muscles of the spine. If the patient doesn't strengthen and balance the muscles, they will not heal, whether the issue is the disc, the SI, or any other lower back problem. There is extensive literature on low back exercise. For an overview, consider Craig Liebenson's new 2006 edition of Rehabilitation of the Spine: A Practitioner's Manual.
I am reminded of a story. A young mother brought her son to Gandhi, and asked him, "Gandhi, would you please tell my son to stop eating sugar, he is rotting his teeth, and ruining his health." Gandhi smiled his inscrutable smile, and told the woman and her son, "Come back next week." The woman returned the next week, enduring the 10-hour bus ride, the dust, and the three-hour wait in line. "Gandhi, would you please tell my son to stop eating sugar." Gandhi sat down with the young boy, and sincerely told him to stop eating sugar, detailing why this was important to him. The woman said, "Thank you, thank you, Mr. Gandhi. Can I ask you one more question? Why did you make us come back a second time?" Gandhi replied, "Oh, last week I was eating sugar."
How many of us really live the chiropractic lifestyle, really "walk the walk?" I have noticed that I am a better exercise coach this year, since I am actually doing the exercises. What little steps could you take with your diet, your exercise, your lifestyle?
A bit more on the specific exercise modalities I have used: Many of you are familiar with Pilates, an old methodology that has experienced a recent revival. Pilates is a series of whole-body exercises, done either on a mat or with specific equipment, that focuses on core strength. Pilates has become so popular that it has become diluted. Many teachers do not really have the training necessary, and it is not always taught correctly, putting backs at risk.
 Anusara yoga is a fairly recent yoga variation. When you get beyond the specific yoga jargon, anusara focuses on isometric co-contraction in specific postures, using multiple muscle groups simultaneously, with an emphasis on optimal alignment. There is a focus on optimal core strength. As an example, I'll contrast my understanding of prone McKenzie extension with the yoga sphinx or cobra. The picture looks the same, but in the anusara yoga versions, the patient would activate and pull in with the lower abdomen, lift with the chest, pull the shoulder blades downward, and keep the head in neutral. I shared one anusara pose, which I have renamed "spine lengthening squat," in my article on pain relief exercises (www.chiroweb.com/archives/23/23/11.html). Anusara yoga requires a strong sense of attention; of being fully present in the body while you move or hold the poses.
Anusara yoga is a fairly recent yoga variation. When you get beyond the specific yoga jargon, anusara focuses on isometric co-contraction in specific postures, using multiple muscle groups simultaneously, with an emphasis on optimal alignment. There is a focus on optimal core strength. As an example, I'll contrast my understanding of prone McKenzie extension with the yoga sphinx or cobra. The picture looks the same, but in the anusara yoga versions, the patient would activate and pull in with the lower abdomen, lift with the chest, pull the shoulder blades downward, and keep the head in neutral. I shared one anusara pose, which I have renamed "spine lengthening squat," in my article on pain relief exercises (www.chiroweb.com/archives/23/23/11.html). Anusara yoga requires a strong sense of attention; of being fully present in the body while you move or hold the poses.
I will close with this thought:
Show up and pay attention. You have the opportunity for 30-40 hours of incredible continuing education each week in your practice. It's only a learning experience if you are fully present. You can go through the motions and help some people. If you are fully awake, you will learn something new every day and get remarkable results.
References
- Yrjama M, Tervonen O, Kurunlahti M, Vanharanta H. Bony vibration stimulation test combined with magnetic resonance imaging. Can discography be replaced? Spine 1997;22(7):808-13.
- Vanharanta H, Ohnmeiss D, Aprill C. Vibration pain provocation can improve the specificity of MRI in the diagnosis of symptomatic lumbar disc rupture. Clin J Pain 1998;14:239-247.
- Vanharanta H, personal communication.
- Explanation of anusara yoga principles by Doug Kellogg. www.doyoga.com/index_therapy_overview.html.
Click here for more information about Marc Heller, DC.





