During our chiropractic training, we are strongly oriented to the mechanics of spinal dysfunction, such as disc-related pains. This article complements the mechanical focus by highlighting the chemistry of disc pain and discussing a biochemical intervention.
I would argue that these designations are a problem, as pain syndromes seen by chiropractors can only be nociceptive or ectopic nociceptive in nature.1 Altered mechanics and inflammation are known to be involved in each, and so arbitrarily referring to spine pain as mechanical is, well, arbitrary, and discounts acknowledged pathophysiological processes. Several years ago, Dr. Geoffrey Bove and I reviewed this information, which helps to explain why, from a mechanistic perspective, discogenic pain is nociceptive and radicular pain is ectopic nociceptive.1
This issue can be better understood by examining the discogenic pain and disc herniation pain process. The relevance of understanding this information is clinically important, as so many patients have disc-related pains, such that 40 percent of chronic back is discogenic and 5 percent is due to disc herniation.2
In order for disc-induced pain to develop, the vertebral endplate must first be disrupted.2-4 The endplate is the weakest link in the disc complex. A normal nucleus and annulus are not damaged by stressful loading activities; however, the endplate is at risk.2-4 Visualizing endplate damage is nearly impossible, so the process must be understood.
Endplate damage is a "mechanical event" that is commonly asymptomatic; however, it leads to the internal disruption of the nucleus, which is an "inflammatory process." We know this because the disruption process has been studied and was outlined in detail at least as early is 1997.4 Bogduk explained that endplate damage turns on disc proteinases, which leads to the enzymatic degradation of the nucleus,4 which is an inflammatory process that leads to an uncoupling of the normal mechanics of the disc.
Matrix Metalloproteinases
Back in 1997, Bogduk described the enzymes as proteinases4 and in his 2005 edition, they were properly referred to as matrix metalloproteinases or MMPs.3 Until very recently, most health care practitioners (DC, MD and DO) would have recognized MMPs by their original names, such as collagenase, elastase, gelatinase and stromelysin.
The pathological process is straightforward. Endplate damage turns on MMPs, which leads to the relentless progressive degradation of the nucleus.4 After the nucleus is degraded, the MMPs then erode the inner annulus, which creates radial fissures.4 In other words, the radial fissures seen on a discogram are generated by MMPs; not by mechanical tears.4 Figure 1 [reprinted with permission from Chirogeek.com] illustrates the discogram grading system.
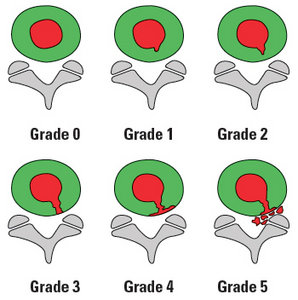 Figure 1: Modified Dallas Discogram
Discogenic pain appears when the outer third of the annulus is breached (grades 3 and 4). The nerve root is directly compromised in a grade 5 discogram. The degradation process can stop at any stage, which is accomplished by anti-inflammatory signaling via tissue inhibitors of metalloproteinases (TIMPs). However, if the MMPs are not inhibited, they will continue to degrade the inner annulus, extend into the outer annulus as radial fissures, and potentially breach the outer annulus and manifest as a frank herniation.
Figure 1: Modified Dallas Discogram
Discogenic pain appears when the outer third of the annulus is breached (grades 3 and 4). The nerve root is directly compromised in a grade 5 discogram. The degradation process can stop at any stage, which is accomplished by anti-inflammatory signaling via tissue inhibitors of metalloproteinases (TIMPs). However, if the MMPs are not inhibited, they will continue to degrade the inner annulus, extend into the outer annulus as radial fissures, and potentially breach the outer annulus and manifest as a frank herniation.
To be clear, in 1997, Bogduk explained that this "is an inflammatory condition that involves degradation of the nuclear matrix and progressive erosion of the annulus."4
Despite the fact that inflammation is responsible for the discogenic pain and disc herniation process, I would not call this pain "inflammatory pain." As stated earlier, the proper terms are nociceptive and ectopic nociceptive pain, respectively.
Inhibition of MMPs
So, the goal should be to inhibit MMPs before they degrade the nucleus and eat into the annulus. Unfortunately, there is no evidence yet as to how to stop the process; although from a preventive perspective, we have indirect evidence from the study of heart disease.
Patients with the metabolic syndrome, type 2 diabetes, hypertension, dyslipidemia and obesity have a generalized elevation of MMPs.5 We could hypothesize that these patients are at greater risk for disc herniation, but is this true? In fact, research has demonstrated that patients with the metabolic syndrome and type 2 diabetes have an increased risk of expressing disc herniation.6-8 Additionally, advanced glycation end products associated with hyperglycemia have been identified as promoters of disc herniation.9-10
While yet to be demonstrated from a therapeutic perspective, this information suggests that disc patients should immediately adopt a low glycemic index / load diet and consider supplementing with nutrients that have blood sugar benefits, such as magnesium, vitamin D, chromium and lipoic acid.
Some may argue that this would not reduce the pain associated with an acutely herniated disc. While this may or may not be true, and likely depends on individuals patients, the naysayers should adopt a different and more appropriate mindset. Why would a patient with an acute inflammatory state knowingly consume foods that are known to augment acute system inflammation immediately upon consumption? Doing this may be one of the dumbest dietary choices we can make.
We now know that high-glycemic foods lead to an immediate postprandial systemic inflammatory surge.11 And this has been studied in lean, healthy individuals, so why should any patient with an acute inflammatory state, like a hot disc, not be alerted to the foods that are known to cause acute systemic inflammation?
Supplements for Acute Discogenic and Disc Herniation Pain
While supplements have yet to be studied specifically for disc herniation, this should not stop us from using supplements. Why is this the case? Because the inflammation of discogenic pain and disc herniation is no different than any other musculoskeletal inflammatory event. For years, proteolytic enzymes have been used to treat acute musculoskeletal injuries, an approach that should employed in discal pain syndromes. The same holds true for botanical anti-inflammatories, especially turmeric and ginger.
And if we look at how humans historically consumed animal products, we realize they left nothing to waste, meaning that they also ate connective tissue and marrow. This means they ate collagen and proteoglycans on a regular basis. From a modern perspective, we can do the same by eating gelatin and taking supplemental glucosamine sulfate and chondroitin sulfate. I would recommend we do this before injuring musculoskeletal tissues; however, if an injury has already occurred, then certainly supplementation should begin afterward.
References
- Bove GM, Seaman DR. "Subclassification of Radicular Pain Using Neurophysiology and Embryology." Dynamic Chiropractic, May 20, 2012.
- Adams M, Bogduk N, Burton K, Dolan P. The Biomechanics of Back Pain. New York: Churchill Livingstone; 2002: p. 78.
- Bogduk N. Clinical Anatomy of the Lumbar Spine and Sacrum. New York: Churchill Livingstone; 2005: p. 198-204.
- Bogduk N, Twomey TL. Clinical Anatomy of the Lumbar Spine. New York: Churchill Livingstone; 1997: p. 1677-173.
- Hopps E, Caimi G. Matrix metalloproteinases in metabolic syndrome. Eur J Intern Med, 2012;23(2):99-104.
- Jhawar BS, Fuchs CS, Colditz GA, Stampfer MJ. Cardiovascular risk factors for physician-diagnosed lumbar disc herniation. Spine J, 2006;6:684-91.
- Sakellaridis N. The influence of diabetes mellitus on lumbar intervertebral disk herniation. Surg Neurol, 2006;66:152-4.
- Sakellaridis N, Androulis A. Influence of diabetes mellitus on cervical intervertebral disc herniation. Clin Neurol Neurosurg, 2008;110:810-2.
- Tsuru M, Nagata K, Jimi A, et al. Effect of AGEs on human disc herniation: intervertebral disc hernia is also effected by AGEs. Kurume Med J, 2002;49(1-2):7-13.
- Jazini E, Sharan AD, Morse LJ, et al. Alterations in magnetic resonance imaging T2 relaxation times of the ovine intervertebral disc due to non-enzymatic glycation. Spine, 2012;37(4):E209-15.
- Seaman DR. Body mass index and musculoskeletal pain: is there a connection? Chiro Man Ther, 2013;21:15. Download for free at www.chiromt.com/content/21/1/15/abstract.
Click here for more information about David Seaman, DC, MS, DABCN.






