Numerous studies suggest low levels of vitamin D in the blood are strongly linked to increased risk of developing multiple sclerosis (MS); and that MS patients with low blood levels of vitamin D (25- hydroxycholecalciferol) are more likely to have greater disability and more disease activity.
The study included 40 people with relapsing-remitting MS. Patients in the control group, who were given 800 IU per day of vitamin D, did not show a reduction in these MS inflammatory markers. For the patients ingesting 10,400 IU of vitamin D per day, when the increase in vitamin D levels in the blood over baseline levels was greater than 18 ng/ml (45 nmol/L) every additional 5 ng/ml (12.5 nmol/L) increase in vitamin D led to a 1 percent decrease in the percentage of IL-17+CD4+ T cells in the blood. Patients taking the low dose did not experience any noticeable changes in the percentages of their T cell subsets.
The hope is that these changes in inflammatory T cell responses translate into a reduced severity of disease, and other clinical trials are underway to determine if that is the case. However, these findings are quite encouraging, especially considering that no significant side effects were reported by MS patients administered the high-dose vitamin D supplementation protocol compared with those taking the low-dose protocol.
 With respect to optimal vitamin D blood levels for MS patients, researchers are still working to determine what range is most beneficial. At the present time, 40-60 ng/ml has been proposed as a target range. This is equivalent to 100-150 nmol/L. Participants taking the high-dose vitamin D protocol reached levels within the proposed target, whereas the group taking the low-dose (800 IU) did not reach the target. It is noteworthy that patients with severe vitamin D deficiency were not included in the study.1
With respect to optimal vitamin D blood levels for MS patients, researchers are still working to determine what range is most beneficial. At the present time, 40-60 ng/ml has been proposed as a target range. This is equivalent to 100-150 nmol/L. Participants taking the high-dose vitamin D protocol reached levels within the proposed target, whereas the group taking the low-dose (800 IU) did not reach the target. It is noteworthy that patients with severe vitamin D deficiency were not included in the study.1
Inflammatory Markers in MS
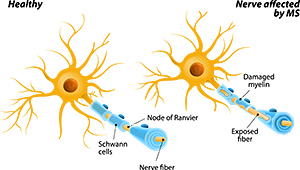
Multiple sclerosis is the most common neurological disease in young adults, afflicting hundreds of thousands of people worldwide. Until recently, researchers had highlighted the role of type 1 and type 2 cytokines in the etiology of MS. The general notion was that a type 1 response (with CD4 T cells of helper type 1, TH1 cells) was associated with a pro-inflammatory, destructive immune reaction, whereas a type 2 response (with TH2 cells) reflected a modulatory, non-pathogenic immune reaction, which may even protect against autoimmune disease caused by TH1-dependent mechanisms.
More recently, it has been shown that IL-23 is an upstream modulator of an important pathogenic signaling pathway in MS. IL-23 is crucially involved in the expansion of cells producing IL-17, and IL-17 is produced by TH cells that are distinct from the traditional TH1 and TH2 cell subsets. This rapidly emerging evidence clearly demonstrates that TH17 cells are indeed a T-helper cell subpopulation distinct in differentiation and function from the TH1 and TH2 subsets described previously.
Of great clinical significance is the fact that a systematic analysis of IL-17-positive cells in the brains of MS patients revealed a significant increase in the number of IL-17+ T cells in the active, rather than the inactive areas of MS lesions. Another critical finding: IL-17 immunoreactivity also could be detected in astrocytes and oligodendrocytes in active areas of MS plaques.
All of these findings have made it increasingly clear that IL-17 is an essential player in MS, and is likely an important target for future therapeutic interventions to improve MS progression and outcomes.2 As such, the discovery that high-dose vitamin D supplementation can downregulate the release of IL-17 in MS patients is of great significance.1
Interleukin-17: A Key Cytokine in MS
IL-17 is a signature cytokine of TH17 (T-helper 17) cells and plays critical roles in host defense against bacterial and fungal infections, as well as in the pathogenesis of autoimmune diseases. IL-17 is highly up-regulated at sites of inflammatory tissues of autoimmune diseases and amplifies the inflammation through synergy with other cytokines, such as TNF (tumor necrosis factor) α. Although IL-17 was originally thought to be produced mainly by TH17 cells, a newly defined T-cell subset with a specific differentiation program and tight regulation, several other cell types (especially innate immune cells) are also important sources for IL-17 production.
Mouse genetic studies have demonstrated a critical role for IL-17 in the pathogenesis of a variety of inflammatory autoimmune diseases, such as RA (rheumatoid arthritis) and MS. Importantly, promising results have been shown in initial clinical trials of monoclonal antibodies against IL-17 or its receptor (IL-17R) to block IL-17-mediated function in treating autoimmune patients with psoriasis, RA and MS.3 Human studies also have shown that IL-17 is overexpressed in patients with Crohn's disease and that IL-17 induces a pro-inflammatory response in this condition.4
Other Vitamin D Studies Involving MS Patients
Presenting at the American Academy of Neurology in 2009, Dr. Jodie Burton revealed the results of a vitamin D trial in MS patients. This study suggests high doses of vitamin D (14,000 IU per day for one year) dramatically cut the relapse rate in people with multiple sclerosis compared to those given only 1,000 IU per day of vitamin D over the same time period.
More specifically, 16 percent of 25 MS patients in the high-dose vitamin D group suffered relapses during the one-year period, compared to 40 percent in the low-dose vitamin D group (24 MS patients). Additionally, patients taking high-dose vitamin D suffered 41 percent fewer relapses than the year before the study began, compared with 17 percent fewer relapses by patients taking typical doses (1,000 IU – the amount typically recommended to MS patients by neurologists). Also encouraging was the fact that patients taking high doses of vitamin D did not suffer any significant side effects.5
Clinical Pearls
Compelling evidence has linked low vitamin D levels with increased risk for MS, and progression of MS in patients suffering from the disease. Our understanding of the importance of vitamin D in immune system modulation continues to unfold with each passing year. Most recently, we have learned vitamin D is capable of downregulating the overexpression of IL-17, a highly implicated cytokine in the pathophysiology of multiple sclerosis.
We have preliminary evidence that high-dose vitamin D supplementation (approx. 10,000-14,000 IU per day) can reduce IL-17 levels and significantly reduce relapses in MS patients. This is indeed encouraging, and suggests neurologists may want to reconsider their usual recommendation of 1,000 IU vitamin D per day for MS patients by increasing this amount to 10,000-14,000 IU per day, for at least the first year.
In these cases, monitoring vitamin D blood levels (25-hydroxycholecalciferol) should be undertaken to ensure a range of 40-60 ng/ml (100-150 nmol/L) is achieved while avoiding vitamin D toxicity, which typically can occur at vitamin D blood levels nearing 100 ng/ml (250 nmol/L).
Complementary health practitioners also should be encouraged to discuss these findings with their MS patients and to follow the results of future clinical trials involving vitamin D administration to MS patients.
References
- Sotirchos ES, Bhargava P, Eckstein C, et al. Safety and immunologic effects of high- vs low-dose cholecalciferol in multiple sclerosis. Neurology, 2016 Jan 26;86(4):382-90.
- Gold R, Luhder F. Interleukin-17 - extended features of a key player in multiple sclerosis. Am J Pathol, 2008;172(1):8-10.
- Zhu S, Qian Y. IL-17/IL-17 receptor system in autoimmune disease: mechanisms and therapeutic potential. Clin Sci, 2012;122(11):487-511.
- Siakavellas SI, Bamias G. Role of the IL-23/Il-17 axis in Crohn's disease. Discov Med, 2012 Oct;14(77):253-62.
- Laino C. "High Doses of Vitamin D Cut MS Relapses." WebMD, April 28, 2009.
Click here for more information about James P. Meschino, DC, MS.





