Dear Dr. Batchelor:
I have been diagnosed with an L5 disc herniation. As a runner, I am very concerned that I will never be able to run again as a result of this condition.
Andrea
Dear Andrea:
Back pain is exceedingly frequent, experienced at some time by up to 80 percent of the general population. Within the running population, however, the figure is somewhere between 80 percent and 90 percent. There are many reasons why the runner tends to suffer from lower back pain more frequently than the nonrunner. Running places three to four times the body weight on each leg during impact. Running strengthens the lower back, but does not do much to increase the strength of the abdominal muscles. The greater the ratio of strength between the abs and the lower back muscles, the greater the stress on the lower back discs. Running on concrete or asphalt increases the stress on the lower back compared to running on wood chips, dirt or a treadmill. Running combined with a leg-length discrepancy and the resultant vertebral misalignment can also increase the susceptibility for suffering from lower back pain.
Diagnosis of low back pain is broad and includes systemic diseases (metastatic cancer), kidney stones, and primary spine disease (disc herniation, degenerative arthritis), all of which refer pain to the low back. More common causes, however, include subluxation, misalignment, sprains, strains and muscle imbalances. Conventional medical treatment regarding back pain is often flawed, frequently painful, and can be exceedingly expensive. Causes of mechanical low back pain include degenerative disc disease, degenerative spondylosis with limitation of range of motion, joint arthropy, herniation and segmental instability. Any activity that increases axial loading on the spine, such as sitting, standing and/or lifting, will exacerbate low back pain. Research has shown that simply running down the road actually exerts less pressure inside the spinal disc space than pressure exerted within the spinal disc from simply sitting in a chair.
Using standard chiropractic techniques, non-disc-related conditions usually respond very quickly, and symptoms usually improve very rapidly. More severe disc conditions, however, generally take two to six times longer to respond than non-disc conditions. Occasionally, surgery is the only option, but most of our disc/back pain patients respond well and return to normal activity. The problem with a disc is that it can pinch or irritate a nerve from the spinal cord, resulting in pain that affects the legs (sciatica). Sciatica can be severe and disabling. If the patient does not have the condition treated and corrected, there is strong physiologic evidence of dysfunction of the spinal segment consisting of the intervertebral disc and its adjoining vertebrae.
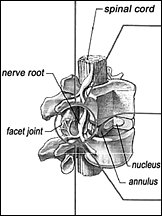
As mentioned earlier, the most difficult back condition to treat involves the disc - specifically, the herniated spinal disc. The structure of a disc is actually very easy to understand. The outer protective ring is called the annulus fibrosis; it protects and encases the nucleus pulposus, the jellylike center. The nucleus is the pivot point upon which the vertebra moves. Increases in intradisc pressure can cause the disc to tear slightly and the nucleus can push into the annulus, putting pressure on sensitive nerves nearby. When the nucleus has completely ruptured through the annulus, this is called a severe and complete disc herniation; it is one of the most difficult back conditions to treat. When the nucleus pushes sideways against the annulus, there will be pain in one leg. When the nucleus pushes posteriorly against the annulus, there will be pain in both legs. We use various chiropractic and orthopedic tests to differentially diagnosis these more severe disc conditions.
Primary disc pain can occur with mechanical strain of the annulus that allows nuclear herniation through radial fissures, and from inflammation following trauma. A healthy disc can become painful if disease in other portions of the spine cause it to bear greater mechanical load and secondarily subject it to excessive strain. It is critical to realize that several mechanisms of pain may coexist and that similar disease processes give varying symptoms. Conventional medicine has two common (although less-than-ideal) options for the treatment of herniated discs: surgery and physical therapy. Recently, tables designed specifically for treating patients with disc conditions have been developed. They are called flexion/distraction tables, and are used to decrease the pressure inside spinal discs. Surgery for disc conditions is not the only treatment that can lead to increased disability: Methods such as extended bed rest or use of high-dose opioids can prolong symptoms and further debilitate patients. Steroids, anti-inflammatory agents and muscle relaxants can fall short of treating underlying problems associated with intervertebral disc lesions. None of these methods relieve pain from neurocompression or from the stimuli associated with prolapsed nucleus pulposus.
Research implies that intradiscal pressure that elevates in a controlled manner plays a role in disc lesions, and now we are learning that lowering intradiscal pressures in a controlled manner plays a role in treating low back pain. New advances centering on the use of decompression, reduction and stabilization produced several important studies on the effect of decompression on intradiscal pressures. The intervertebral disc and the two articulating joints above and below form a spinal segment with limited range of movement when isolated. Several spinal segments together, however, can produce large ranges of sagittal and coronal plane movement. The disc provides the main strength and stiffness, and consists of a thick annular wall that attaches through cartilaginous plates to the vertebral bodies, while the inner nucleus pulposus behaves hydrostatically as a viscous fluid, changing shape in response to body position - in effect, acting like a joint. The nucleus receives axial loads and redistributes the load centripetally to the surrounding annulus, but aging reduces the vascularity of the outer annulus and cartilaginous plates to a few small vessels.
Flexion and lateral bending increase intradiscal pressure, while resting pressures are lowest in supine and prone positions, lower in standing than sitting, and very low in activities of lumbar extension and rotation. Intradiscal pressure is greater when running uphill than downhill because of the lumbar flexion that occurs as you run uphill. Running downhill causes lumbar extension, which places more stress on the joints of the lower vertebra, but not on the disc. Exercise programs and ergonomic techniques emphasize the maintenance of lordosis to maintain decreased pressures and help prevent injury. Decompressing the disc space through positioning of the patient promotes tissue healing, as evidenced by MRI-documented reductions in the size and extent of herniations.
Smoking, previous surgery, chronic use of narcotic or steroid medications, obesity, and large amounts of daily caffeine can have negative influences on the treatment.
Treatment frequency is based on diagnosis. For example, a patient with a herniated disc will, on average, be treated daily for two weeks, then three times per week for two weeks, with re-evaluation weekly.
Over the years, I have noticed that runners tend to be more keenly perceptive of how their bodies function than nonrunners. I enjoy treating runners because they ask many questions, demand science-based answers, and tend to appreciate a doctor who has the same interests and goals as they do.
Daniel Batchelor, DC
Roswell, Georgia
(770) 992-2002
Click here for previous articles by Daniel Batchelor, DC.