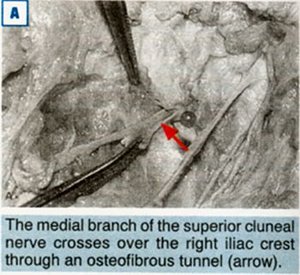
Lu et al.1 described for the first time the anatomic relationship of the superior cluneal nerve to the posterior iliac crest and thoracolumbar fascia. They dissected 15 cadavers and found that the medial branch of the superior cluneal nerve is confined within a tunnel consisting of the thoracolumbar fascia and the superior rim of the iliac crest as the nerve passes over the iliac crest (see Figures 1A and 1B). The location is 7-8 cm lateral to the midline (sacral spinouses) on the iliac crest just lateral and superior to the posterior superior iliac spine (PSIS). "The medial branch of the superior cluneal nerve passes superficially over the iliac crest, and is covered by two layers of dense fibrous fascia."1
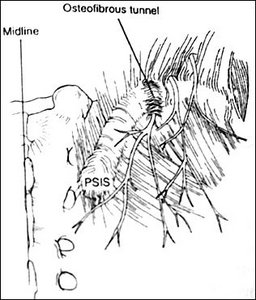
B. A diagram showing the site of the osteofibrous tunnel for the medial branch of the superior cluneal nerve.
If this pain location was due to a facet syndrome, the facet affecting the superior cluneal nerves would be at the level of T12, L1 or L2, whose nerves come out through the lumbosacral fascia at the lateral origin of the sacrospinalis muscles and cross over the dorsal part of the posterior iliac crest.2 Pressure over the particular facet involved might be sensitive if it was a facet syndrome, and the area would hopefully be relieved if the involved facet were adjusted. The trigger point involved at this area is supposed to correspond to the insertion of the iliolumbar ligament, except for the fact that the insertion of the iliolumbar ligament is on the anterior aspect of the iliac crest and cannot be palpated.3 However, treatment of a trigger point in the area may offer relief due to its effect on the cluneal nerve.
The medical branch of the superior cluneal nerve might be restricted in its osteofibrous tunnel against the iliac crest, just as osteofibrous tunnels affect other nerves such as the tarsal tunnel or carpal tunnel syndrome, among others. Active release should clear up the problem. The area will palpate as thickened, tender tissue, and there might be a positive Tinel's sign. The adhesion affecting the nerve could be freed by using pressure over the area as the patient (in the side position) actively flexes the thigh. Due to the entrapment in the fascial layers, the fascia should first be palpated as to the direction of the fascial barrier, which will determine the direction of the tissue pressure.
References
- Lu J, Ebraheim NA, Huntoon M, et al. Anatomic considerations of superior cluneal nerve at posterior iliac crest region. Clin Orth & Rel Res 1998;347:224-228.
- Drury BJ. Clinical evaluation of back and leg pain due to irritation of the superior cluneal nerve. J Bone Joint Surg 1967;49A(1):199. Abstract.
- Maigne JY, Maigne R. Trigger point of the posterior iliac crest: painful iliolumbar ligament insertion or cutaneous dorsal ramus pain? An anatomic study. Arch Phys Med Rehabil 1991;72:734-737.
Warren I. Hammer, MS, DC, DABCO
Norwalk, Connecticut
Click here for previous articles by Warren Hammer, MS, DC, DABCO.





