Editor's note: Part one of this article appeared in the Dec. 16, 2004 issue.
Rehabilitation of the Knee: Restoring Static Restraints, Dynamic Restraints, Proprioception and Sport-Specific Skills
The static restraints of the knee are the ligaments and bony architecture that limit movement.The dynamic restraints of the knee are the muscles and tendons that surround the knee. These muscles and tendons maintain joint position and react to changing loads and forces. Post-surgery rehabilitation depends on restoring the function of these dynamic restraints, with the main focus on restoring flexibility and strength to the hamstring and quadriceps musculature. During the initial phases of rehabilitation, isometric strength-training exercises are implemented, whereby the muscle neither shortens nor elongates, but force is generated. A straight leg raise is an example of an isometric strength training exercise for the quadriceps musculature. Later in the postoperative rehabilitation phase, exercises will be conducted to develop eccentric strength (whereby the muscle elongates to decelerate a particular movement) and concentric strength (whereby the muscle shortens to promote a particular movement). An example of an eccentric exercise is step-downs off of a two-inch box with the good leg. During a step-down, the quadriceps of the injured leg eccentrically fires to decelerate and control leg flexion; simultaneously, the gluteus musculature of the injured leg fires to stabilize the pelvis, so the body doesn't tilt to the side of the uninjured leg that is stepping down. An example of a concentric strengthening exercise is forward step-ups, whereby the quadriceps concentrically contract to force the leg to extend. Rehabilitation of the dynamic restraints will aid in taking stress off of the repaired ACL, preventing re-injury.
Proprioception is best defined as reception of sensory input from mechanoreceptors (specialized cells located in the skin, muscles, tendons, ligaments, and joints), the visual field, and the vestibular system. This sensory input is processed at the spinal cord, then at the mid-brain or the more complex cerebral region. A reflex or motor response is generated and then regulated until the desired movement is attained. There are three main types of reflexes, the fastest being the involuntary knee-jerk reflex, which involves no brain processing or thought. The second fastest reflex involves thought processing through the mid-brain, and the slowest reflex involves more involved thought processing in the cerebrum. Repetitive balance and movement drills can transfer reflexes that initially involve complex sensory processing in the cerebrum to the mid-brain, leading to faster, more precise movement patterns. Proprioception training involves retraining and fine-tuning reflexes and movement patterns through balance drills, agility drills, plyometric jumping drills, and sport-specific training. Proprioception training will increase the state of readiness of the knee re-injuring joint, decreasing the chance of reinjuring the ACL upon return to sport.
Full functional rehabilitation of the knee depends on restoring static stability, dynamic stability, and proprioception. The rehabilitation program should be individualized with regards to the patient's coordination, desire, and specific sport.
Weeks 0-2
The goals of the first two weeks of postoperative rehabilitation are to reduce swelling, restore full range of motion in extension and flexion, ambulate without the use of crutches, and sit down and stand from a seated position. Straight leg raises, side raises/abduction exercises, and assisted leg extensions to full extension (with the help of the therapist or the opposite foot) are good exercises to initiate muscle firing of the quadriceps and gluteus musculature.
Muscles located in and above the back of the thigh, the hamstrings and gluteus structures, stabilize the pelvis during ambulation and squatting-type movements. Two exercises that are instrumental in returning coordinated strength to the leg are isometric co-contractions of the hamstring and quadriceps musculature; and properly performed quarter squats and full chair squats. The co-contractions should initially be conducted at 30 degrees of flexion, progressing at 10-degree intervals up to 90 degrees. Squats should be conducted at the patient's tolerable range of motion in a controlled manner. During the squat, the patient should focus on squeezing the hamstrings and gluteus musculature during the downward movement of the squat and keep a vertical shin angle; these two actions will prevent the patient from leaning forward and placing undue stress on the knee joint. As the patient squats down, the quadriceps musculature fires to decelerate flexion of the leg, while the hamstring and gluteus musculature fire to decelerate the pelvis from rotating forward. The hamstring musculature also aids the reconstructed ACL in its check-rein function on the tibia. These exercises are crucial in developing the coordinated muscular activity of the hamstring, gluteus and quadriceps musculature that is necessary for a normal walking gait during full weight-bearing on a flat surface, as well as for walking up and down stairs and getting into a seated position.
Step-downs (Figure 6A) are another useful exercise that can be included in the second week of postoperative rehabilitation. For this exercise, the patient stands with both legs on a designated raised surface and then steps down to the ground with the non-injured leg. These exercises should be conducted in front of a mirror to ensure proper technique.
Apprehension in flexing the injured leg or weakness in the gluteus musculature on the same side will cause the patient's pelvis to drop down to the side of the leg that is stepping down. Correct technique of step-downs is necessary for the patient to maintain hip stabilization, prevent pelvis drop, and ensure proper co-contraction of the hamstring and quadriceps musculature of the injured leg, to achieve a controlled leg flexion as the other foot touches the ground surface. Step-downs should commence at two inches off the ground for 25 controlled repetitions. The step-down height can be increased to four, six, and eventually eight inches as the patient regains motor control of the hip stabilizers, gluteus and hamstring musculature, as well as the decelerator of leg flexion, the quadriceps musculature.
After ACL repair, the sutures are usually removed between 10 days and two weeks post-surgery. Once the wound heals, pool therapy can begin. Specialized pool routines are recommended for total body training, with an emphasis on hip and knee flexion and extension movements, as well as core strength exercises to include all of the muscles involved in stabilizing the torso from the hips to the shoulder. The patient holds floatation bars while conducting various movements in the pool to improve the coordinated strength of the hip stabilizers, knee extensors and flexors, as well as the core strength musculature.
After 115 degrees of leg flexion is attained, stationary cycling can commence to increase range of motion of the knee joint, as well as provide light endurance exercise. Other exercises that can be used to increase range of motion and muscle coordination are swimming and the elliptical machine.
All of the above exercises, included in the second week of the postoperative rehabilitation phase, should be conducted to the patient's tolerance and in a controlled setting. If swelling occurs or if there is decreased range of motion in the knee joint, the progression of the rehabilitation phase should be slowed down, the range of motion restored, and the swelling reduced.
Weeks 3-5
In weeks 3-5, functional exercises can be added to the rehabilitation routine. The following exercises are recommended:
- Balance star drills on a flat surface - balance while reaching forward with the good leg or opposite arm.
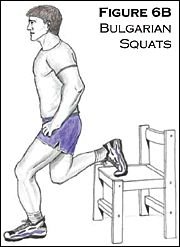
- Bulgarian squats - with the good leg up on a bench/chair, perform the squat with the injured leg (Figure 6B).
- Pelvic bridge - lying on the back, legs flexed to 90 degrees, lift the buttocks off of the floor while squeezing the glutes and the hamstrings.
- Balance drills on a disco-sit/curved seat cushion.
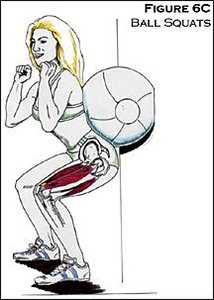
- Ball squats without weights, and later, with weights held during the squat (Figure 6C).
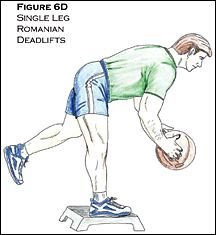
- Single-leg Romanian deadlifts - on a step box, bend forward from the trunk while holding a weighted ball with both hands in front, and balance on the deconditioned leg (Figure 6D).
- Leg presses - single leg.
- Abduction, adduction, single-leg extensions, calf raises.
- Ball tosses while balancing on a balance board.
- Lunges.
- Exercise ball hamstring curls.
- Towel stretches and standing extension stretches with resistive tubing.
Delayed-onset muscle soreness is expected. If there is normal range of motion, no immediate swelling, and muscle pain dissipates in two to three days, the patient can continue to progress with the rehabilitation routine.
Weeks 6-8
- Progress to heavier weights with the above exercises.
- Continue towel stretches and flexible band stretches to maintain and increase range of motion of the knee in both flexion and extension.
- Proprioception drills - e.g., wobble board exercises balancing on two legs, balancing on one leg, ball tosses while balancing; done with the eyes closed for advanced drills.
Weeks 8-11
- Romanian deadlifts; and
- Light sport-specific training - e.g., a basketball player shooting free throws or conducting passing drills.
Week 12
If the patient has full range of motion and strength of the musculature surrounding the knee, he or she may start a running program: treadmill running for 10 to 15 minutes, level surface running on cement for 20-30 minutes, hill running, sprinting, figure 8s, side-sliding, start-and-stop shuttle runs, and 45-degree cutting. Jumping drills can teach the athlete how to land softly while sitting back and incorporating the hamstring and gluteus musculature. These agility drills can be progressed as tolerated.
4-6 Months
The patient can return to full light-sport participation, assuming full range of motion, 90 percent strength of the hamstring and quadriceps musculature (as compared to the healthy leg), and success in conducting all of the agility drills with no pain or swelling.
The therapist should explain to the patient that while it is acceptable to return to full light-sport specific training, it can take up to three months of participation to regain the complex movement patterns of the particular sport. It may take seven months to a year for "ligamentization" of the grafted tissue, whereby the grafted tissue becomes almost identical in its properties to the original anterior cruciate ligament.
Therapeutic Restoration of Soft-Tissue and Joint Motion
Hands-on treatment of the repaired ACL can commence after the sutures are removed and the wound is healed - approximately two weeks post-surgery. This treatment consists of:
- specific muscle work, including active release technique, to free up soft-tissue motion of the surrounding knee musculature, helping to restore normal range of motion of the knee in flexion and extension;
- ultrasound and electric muscle stimulation combo therapy to break up scar tissue and restore normal muscle tone; and
- patella mobilization techniques.
The above treatment protocols are useful in breaking up scar tissue and restoring proper joint and soft- tissue range of motion. This will aid in speeding up the postoperative rehabilitation phase.
Good communication among practitioners and repeated patient follow-ups are crucial in creating and maintaining the optimum treatment protocol for pre- and post-surgery rehabilitation of the anterior cruciate ligament, allowing the athlete to return to his or her sport more quickly and with less risk of re-injury.
Author's note: This paper was made possible with the help and expertise of Keith Callanan, MPT, CSCS, and Bill Knowles, ATC, CSCS.
Resources
- Shelbourne DK, Rowdon GA. Anterior cruciate ligament injury. The complete athlete. Sports Med 1994;17(2) 132-140.
- Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RM. Tendon-healing in a bone tunnel. J Bone Joint Surg 1993;75A:1795-1803.
- O'Neill, Daniel F. New Hampshire Knee Center, The 1st Week Post-Op 2003.
- Rinsberg MA, Mork M, Jenssen HK, Holm I. Design and implementation of a neuromuscular training program following anterior cruciate ligament reconstruction. J of Orthopedic and Sports Physical Therapy 2001;31(11):620-631.
- Hewett TE, Paterno MV, Myer GD. Strategies for enhancing proprioception and neuromuscular control of the knee. Clinical Orthopaedics and Related Research 2002;402:76-94.
- Bill Knowles ATC, CSCS, director of iSPORT at the Vermont Orthopaedic Clinic, Rutland, Vt.
- Keith Callanan, MPT, owner of Elite Sports. Inc., Stoughton, Ma.
- Amiel D, Kleiner JB, Roux RD, Harwood FL, Akeson WH. The phenomenon of "ligamentization": anterior cruciate ligament reconstuction with autogenous patellar tendon. J of Orthopaedic Research 1986;(4):162-172.
- Reid D. Sport Injury Assessment and Rehabilitation, Churchill Livingston International, 1992.
- Norman SW. The Knee, 1994.