Vertebral osteomyelitis, aka. spine infection or septic discitis, is an infection of the disc space that usually involves the discovertebral junction and can involve the epidural space, posterior elements and paraspinal soft tissues.1-3 Many different organisms can be the causative agent for an osteomyelitis; however, staphylococcus aureus is the most common, accounting for up to 90 percent of suppurative infections.
 It has been reported that spinal involvement can account for 2 percent to 4 percent of all cases of osteomyelitis.1-3 The highest incidence occurs in males in the fifth and sixth decade of life, although infants, children and the elderly can be affected. Vertebral osteomyelitis is most commonly found in the lumbar spine, and then in the thoracic and cervical spine. It most commonly affects the vertebral body, not the disc space.3,4 It is common for the patient to report a recent infection (urinary tract, respiratory, skin), recent surgery (including dental work) or other recent medical procedures that involve instrumentation.2,3
It has been reported that spinal involvement can account for 2 percent to 4 percent of all cases of osteomyelitis.1-3 The highest incidence occurs in males in the fifth and sixth decade of life, although infants, children and the elderly can be affected. Vertebral osteomyelitis is most commonly found in the lumbar spine, and then in the thoracic and cervical spine. It most commonly affects the vertebral body, not the disc space.3,4 It is common for the patient to report a recent infection (urinary tract, respiratory, skin), recent surgery (including dental work) or other recent medical procedures that involve instrumentation.2,3
Clinically, the patient presents with an insidious onset of back pain, with or without a fever.1-3 The pain may be localized, exasperated by movement, and throb while at rest. In addition, there may be neurologic findings with radicular, meningeal or spinal-cord involvement.1-3 The patient also may present with general fatigue, malaise and weight loss, and the back pain may be acute or chronic in nature. The patient may present anywhere from two weeks to six months following the initial onset of symptoms.1 Laboratory investigation will demonstrate an increased erythrocyte sedimentation rate (ESR), but nothing specific to indicate an infection.2,3
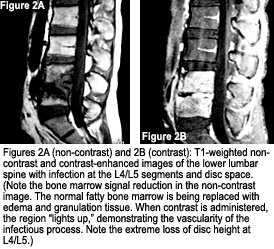
Plain-film radiographs will be indicated in the patient presentation described above. The findings can be variable and dependent upon the aggressiveness of the organism, resistance of the host and extent of involvement. Typical plain-film findings consist of: loss of intervertebral disc height; irregular vertebral endplates on both or one side of the disc; lytic destruction of the vertebral body, with or without collapse; kyphotic deformity; and paravertebral mass representing an abscess.2,3 Osteomyelitis from tuberculosis can have some additional plain-film findings, including sclerosis of the endplates and soft-tissue calcifications. The calcifications can be seen at the infection site, as well as within lymph nodes, the kidney and psoas muscle.1-4 In the early stages of the infection, plain films can be normal or the findings can resemble degenerative disc disease. Order advance imaging within two weeks if the patient is not responding to treatment. Although plain-film findings may suggest the diagnosis of vertebral osteomyelitis, magnetic resonance imaging is the modality of choice for confirmation.1-4
 Once the diagnosis has been made, treatment can be initiated. Nonsurgical management is indicated for patients with minimal or no neurological deficits and no significant kyphotic deformity.5 It is imperative that the patient receive antibiotic therapy to destroy the organisms initiating the infection. This is done either orally or intravenously, depending upon the stage of the infection and health of the patient.1-3 Often, antibiotic therapy is initiated while the actual organism is being cultured for identification. This is done because of the high incidence of staphylococcus aureus as the underlying organism. If a different organism such as mycobacterium tuberculosis is identified, the course of therapy is altered and other medications are initiated. In the case of tuberculosis, antibiotic therapy can last six to 12 months to completely eliminate the organism from the body.1 When the patient develops neurologic findings with considerable damage to the disc and vertebral body, surgical decompression is typically performed, with the primary goal to improve the neurologic deficit, decrease the kyphosis and provide stabilization with bony fusion.5
Once the diagnosis has been made, treatment can be initiated. Nonsurgical management is indicated for patients with minimal or no neurological deficits and no significant kyphotic deformity.5 It is imperative that the patient receive antibiotic therapy to destroy the organisms initiating the infection. This is done either orally or intravenously, depending upon the stage of the infection and health of the patient.1-3 Often, antibiotic therapy is initiated while the actual organism is being cultured for identification. This is done because of the high incidence of staphylococcus aureus as the underlying organism. If a different organism such as mycobacterium tuberculosis is identified, the course of therapy is altered and other medications are initiated. In the case of tuberculosis, antibiotic therapy can last six to 12 months to completely eliminate the organism from the body.1 When the patient develops neurologic findings with considerable damage to the disc and vertebral body, surgical decompression is typically performed, with the primary goal to improve the neurologic deficit, decrease the kyphosis and provide stabilization with bony fusion.5
Although spinal infections are not as common as appendicular skeletal infection, it is important to recognize vertebral osteomyelitis as a cause of back pain. In addition, being aware of the image findings, the appropriate modality to make the diagnosis and the expected therapy the patient will endure will assist us in managing our patients properly.
References
- Hopkinson N, Stevenson J, Benjamin S. A case ascertainment study of septic discitis: clinical, microbiological and radiological features. Q J Med, 2001:94;465-70.
- Resnick D, Niwayama G. Diagnosis of Bone and Joint Disorders, 3rd ed. Philadelphia: W.B. Saunders, 1995.
- Yochum T, Rowe L. Essentials of Skeletal Radiology, 3rd edition, Baltimore: Williams & Wilkins, 2005.
- De Vuyst D, Vanhoenacker F, Gielen J, et al. Imaging features of musculoskeletal tuberculosis. ER, August 2003;13(8):1809-19.
- Rezai A, Woo H, Errico T, Cooper P. Contemporary management of spinal osteomyelitis. Neurosurgery, May 1999;44(5):1018-25.




