I was fortunate enough to join 750 other practitioners and scientists at the First International Fascial Research Congress, held in Boston in October. This was an amazing event, bringing together scientists who have studied various aspects of soft tissue and fascia with the clinicians who have interest in these issues.
Why Do Fusions Fail?
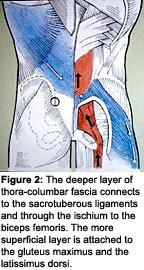
 Why do fusions fail? One answer to this puzzle was provided by Serge Gravcovetsky, PhD. Dr. Gravcovetsky was one of the first to emphasize the importance of the thoracolumbar fascia (TLF).1 Deep fascia lines the low back and is continuous with the deep fascia of the whole trunk. The TLF is a strong sheath that connects the latissimus dorsi to the opposite gluteus maximus (Figure 1). This fascia overlies the lumbar spine and is strongly attached to the sacrum and connects down through the sacrotuberous ligament to the ischium where the biceps femoris begins (Figure 2).
Why do fusions fail? One answer to this puzzle was provided by Serge Gravcovetsky, PhD. Dr. Gravcovetsky was one of the first to emphasize the importance of the thoracolumbar fascia (TLF).1 Deep fascia lines the low back and is continuous with the deep fascia of the whole trunk. The TLF is a strong sheath that connects the latissimus dorsi to the opposite gluteus maximus (Figure 1). This fascia overlies the lumbar spine and is strongly attached to the sacrum and connects down through the sacrotuberous ligament to the ischium where the biceps femoris begins (Figure 2).
The transverse abdominus stabilizes the lumbar spine by its pull through this fascia. Andry Vleeming, editor of a 2007 edition of his text, Movement, Stability, and Lumbopelvic Pain,2 emphasized the understanding of these muscular and fascial connections and how they affect function. Major lumbar surgery (including fusion) cuts this layer of fascia. Without this layer of fascial reinforcement for the musculature, there can be no functional spinal stability. So the surgeon, who has tried to create structural stability via the fusion, has created an unintended consequence of severe functional instability, which is virtually untreatable. Is it any wonder that up to 60 percent of fusions have suboptimal outcomes?
 Why is this fascial layer so important? It's about levers. The deep spinal musculature is too close to the center of movement to have proper leverage to extend the spine and hold us upright. It's the more posterior thoracolumbar fascia, which is pre-stressed (or held in tension by the actions of the TA) and provides the reinforcement for the other muscles to allow us to stay upright.3 We heard a fascinating history of science lecture, which shared with us the contortions that the earlier spinal researchers went through to try to understand and explain the engineering of the spine, before they realized the importance of the thoracolumbar fascia. Dr. P. Huijing showed a series of experiments, using various tendons of the extensor digitorum muscles to show how powerfully the fascia reinforces the muscles. He titled his talk, "Muscle as a Collagen Fiber Reinforced Composite."
Why is this fascial layer so important? It's about levers. The deep spinal musculature is too close to the center of movement to have proper leverage to extend the spine and hold us upright. It's the more posterior thoracolumbar fascia, which is pre-stressed (or held in tension by the actions of the TA) and provides the reinforcement for the other muscles to allow us to stay upright.3 We heard a fascinating history of science lecture, which shared with us the contortions that the earlier spinal researchers went through to try to understand and explain the engineering of the spine, before they realized the importance of the thoracolumbar fascia. Dr. P. Huijing showed a series of experiments, using various tendons of the extensor digitorum muscles to show how powerfully the fascia reinforces the muscles. He titled his talk, "Muscle as a Collagen Fiber Reinforced Composite."
The importance of the "beltline" was further reinforced by a question that Diane Lee, PT, asked the scientists. She outlined a series of cases, postpartum, in which the women had developed a "diastasis recti" - a separation between the two rectus abdominal muscles. She showed ultrasound movies of these women's musculature. In a subset of them, even when they were successfully trained to isolate the transverse abs, they continued to have lower back pain. Her well-grounded speculation was that the abdominal midline connective tissue had become so stretched and so loose that it no longer provided a good anchor for the TA. Thus, this muscle became ineffective in stabilizing the lumbar spine.
This could be seen as an anterior version of what I just described above with the effects of major lumbar surgery on the thoracolumbar fascia. When the key musculature responsible for stability doesn't have a good stiff material to pull against, it becomes ineffective and inefficient. This led to another understanding I came away with: The fascia has places where it is supposed to be "stiff." Soft-tissue workers are always trying to create length to release tissues. Sometimes, the key to function is the inherent stiffness of the connective tissues.
Stability and Mobility
Dr. Gracovetsky and other speakers pointed out that we shouldn't concentrate on stabi-lity without considering mobility. He modeled how the contributions of the musculature and the fascia to low back stability vary with positioning (with changes in the lumbar lordosis). He pointed out that the spine is designed for an ever-changing symphony of interaction, with different muscles and fascial layers being called upon in different movements. When we bend forward at a certain point, the lumbar extensors completely relax (the flexion-relaxation phenomena), and we are supported by the elastic quality of the muscles, ligaments and fascia of the back. He pointed out that the more energy-efficient way to bend forward is to leave the lumbar spine flexed, allowing the fascia (a passive tissue) to store the energy that was used to stretch it and then return that energy while coming back up from bending over. He illustrated this by showing a toddler bending over. The toddler bends like a person with back pain while maintaining their lordosis because their fascia and bones are not yet well-developed. They have to maintain a lumbar lordosis, which uses the musculature to provide the return from flexion. The lumbar musculature being closer to the center of movement is not as efficient at energy storage and return as the more posterior fascia; so, the muscles fatigue when being repetitively used to come out of flexion.
I will admit to being terribly confused by this. I teach my patients to bend at their knees to maintain their lordosis. As a lumbar pain sufferer myself, I bend like someone with back pain, maintaining my lumbar lordosis. I distinctly remember working with my gardener, removing rocks from my pasture. I tried to show him how to "properly" lift the rocks. He tried it my way for a couple of minutes and then said, "That makes my back tired." He went back to bending with full-trunk flexion, over and over, with no apparent negative effects. I don't know what conclusions to draw from this; I don't know exactly how to train my patients with this new knowledge. What I do know is that we need to emphasize training and utilize multiple muscle groups, in multiple different positions, to optimize real-life function.
Trigger-Point Biochemistry
When I was in school many years ago, we were taught that trigger points could be palpated, but that no one had been able to define their difference chemically or histologically. Recent research has clearly delineated chemical differences in an active trigger point, a latent trigger point and normal tissue. This elegant work was done by Jay Shah, PhD, DO, a physiatrist who used in vivo microdialysis using 30-gauge, specially designed needles to evaluate the area.4 (The reference below is an older article on the development of this technology. I don't think this new work on the upper trapezius has been published yet.)
This work probably required the combination of the trained hands of a manual practitioner with the thinking of a scientist. First, Shah had to find the exact center of the trigger point, where the twitch response occurred. He inserted his hollow needles, connected to a pump that filled the area with saline. The needle had another orifice, connected to a vacuum pump, that pulled the fluid, now mixed with biochemicals, from the exact area where the needle was inserted into a chemical analyzer.
They found very consistent results. The active trigger points showed elevations of substance P and other inflammatory mediators, chemicals known to be associated with pain. One of the interesting asides was that while leaving the needle in the spot, these chemical levels rapidly dropped toward normal levels over several minutes. This showed a therapeutic effect of the needle trigger point, although therapy was not the goal of the experiment.
I could go on and on, but I have a general space limit in these articles. I suspect that the importance of connective tissue or fascia is not primarily due to its nerve supply, its being a direct cause of pain or to any contractile elements directly within it. Fascia is critical as the interconnector. Pre-stressed fascia, a viscoelastic material, provides the strength and stiffness to support and reinforce the bones, ligaments and muscles. Its failure and/or its tightness prevents the whole of the musculoskeletal system from working effectively. The surgeon or pain doc fails when they define pain narrowly by just identifying the obvious pain generator. The chiropractor fails when they treat only with joint manipulation based on a narrow view of subluxation. We are all the blind men with the elephant.
Look more broadly and you will potentially be able to help more of your difficult patients. I continue to believe that we in this profession need to define ourselves extensively with the triangle of manipulation, soft tissue and rehab, serving as a stable platform for the best of chiropractic care.
Reference
- Gracovetsky S, Kary M, Levy S, et al. Analysis of spinal and muscular activity during flexion/extension and free lifts. Spine, Dec. 1990;15(12):1333-9.
- Vleeming A. Movement, Stability and Lumbo-Pelvic Pain. Churchill-Livingston, 2007. For detailed description of the text go to: www.elsevier.com/wps/find/bookdescription.cws_home /710631/description#description.
- Barker PJ, Briggs CA. Attachments of the posterior layer of lumbar fascia. Spine, 1999;24(17):1757-64.
- Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J Appl Physiol, Nov. 2005;99(5):1977-84.
Click here for more information about Marc Heller, DC.





