I think back to when I was going through chiropractic school outpatient clinic. I was embarrassed to have my family and friends come in for treatment because initial evaluations took three hours to complete.
All of these processes and getting them signed off by the clinician took an unreasonable amount of time. I remember doing the range-of-motion testing haphazardly and just enough for the clinician to let me commence treatment. After all, wasn't I there to provide treatment? I didn't put much credence into measuring range of motion in joints that were not involved in the primary complaint.
Looking back, I was gravely wrong with this approach, but I just didn't know what I didn't know. Fast-forward 14 years and I realize now how vital it is to look at range of motion in both a systemic and an isolated way to direct care. Nothing gives my treatment plan more teeth than testing range of motion (after ruling out red flags, of course).
No More Static Exams First
In school I was taught to lay someone down to initiate my evaluation. I quickly realized in practice that putting someone in a static, non-weight-bearing posture was not getting me good information. Static examinations have their place, but not until after a movement assessment looks at the system as a whole.
 Figure 1. The base of my treatment philosophy is breaking down dysfunctional movement patterns into a joint, neurological or soft-tissue problem as the main contributor.
Looking at the neuromusculoskeletal system as a whole is truly the keys to the kingdom. This type of movement assessment is analogous to taking someone's blood pressure. We use blood pressure as a screening tool to see if there is an underlying problem that needs further evaluation. If the screen comes out abnormal (e.g., 220/160), we then search for the cause.
Figure 1. The base of my treatment philosophy is breaking down dysfunctional movement patterns into a joint, neurological or soft-tissue problem as the main contributor.
Looking at the neuromusculoskeletal system as a whole is truly the keys to the kingdom. This type of movement assessment is analogous to taking someone's blood pressure. We use blood pressure as a screening tool to see if there is an underlying problem that needs further evaluation. If the screen comes out abnormal (e.g., 220/160), we then search for the cause.
I think of my movement assessments in much the same way. In fact, I look at range-of-motion testing this way as well. If the test is abnormal in a weight-bearing posture, then I look at it non-weight-bearing to see if there is change. Ultimately, this information allows me to break down the movement dysfunction into three distinct categories:
- Joint Issue – Is the joint fixated and needs to be manipulated?
- Soft Tissue – Are soft-tissue structures truly shortened and need to be lengthened?
- Neurological – Is the brain not communicating with the tissue well or asking muscles to tighten for artificial stability?
Understanding how a person moves in space will help identify areas that need to be mobilized, stabilized or strengthened. Figure 1 shows my progressions from assessment through treatment. Notice the base of the treatment is assessment, which gets broken down into the three components or silos (joint, neurologic, soft tissue). (Figure 2)
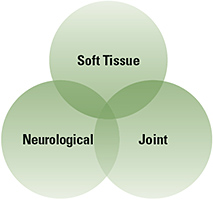 Figure 2. There is no treatment to one of the three silos without overlap into the other two silos.
The power of understanding where most of the dysfunction is coming from allows me to maximize my treatment in the office. In addition, knowing what silo is the common denominator gives me confidence in prescribing a home exercise program. For example, if I have a patient presenting with lower back pain who can't touch their toes during the movement assessment because their hamstrings are too tight, I will prescribe foam rolling and stretching for their hamstrings with lengthening (eccentric) exercises to groove the pattern.
Figure 2. There is no treatment to one of the three silos without overlap into the other two silos.
The power of understanding where most of the dysfunction is coming from allows me to maximize my treatment in the office. In addition, knowing what silo is the common denominator gives me confidence in prescribing a home exercise program. For example, if I have a patient presenting with lower back pain who can't touch their toes during the movement assessment because their hamstrings are too tight, I will prescribe foam rolling and stretching for their hamstrings with lengthening (eccentric) exercises to groove the pattern.
What is grooving the pattern? In my opinion, anytime we put more mobility into the system, we have to apply some resistance training to let the brain adapt this new mobility. Without this crucial step, the brain will just begin to tighten the structures again, searching for stability through muscle tightness. I prefer to use eccentric (lengthening) exercises to accomplish this task. They give resistance while under length to give the brain a chance to adapt to the new movement.
In future articles, I will break down certain areas of the body and conditions and discuss how I attack them from one of the three silos.
Dr. Ed Le Cara recently sold his practice of 14 years in Northern California and relocated to Dallas, Texas. He is the director of athletic training at The Kinetik Chain and the director of trans global education at RockTape, Inc. You can contact him by email at
or Twitter / Instagram (@drlecara) with questions and comments regarding this article.




