Chronic pain is at epidemic levels. The CDC estimates that 50 million Americans, just over 20 percent of the adult population, have chronic pain.1 About 20 million of them have "high-impact chronic pain" – pain severe enough that it frequently limits life or work activities.
Managing Chronic Pain: Where Opioid Therapy Has Gotten Us
Opioid therapy became a standard approach to managing chronic musculoskeletal pain despite a lack of high-quality data on benefits and harms.8 Even though there is a heightened awareness of the opioid crisis, the use and abuse of these drugs has been only moderately reduced. Many patients still receive opioids for chronic musculoskeletal pain, and more than 21 percent of patients who are prescribed opioids for chronic pain misuse them.10
 Krebs and his research team compared opioid vs. non-opioid medications over 12 months.5 Two hundred-forty patients with moderate to severe chronic low back pain, or hip or knee osteoarthritis pain, participated. Opioids and non-opioids both reduced pain from baseline pain intensity scores; but opioids failed to provide better pain relief than the non-opioids at three, six, nine or 12 months.
Krebs and his research team compared opioid vs. non-opioid medications over 12 months.5 Two hundred-forty patients with moderate to severe chronic low back pain, or hip or knee osteoarthritis pain, participated. Opioids and non-opioids both reduced pain from baseline pain intensity scores; but opioids failed to provide better pain relief than the non-opioids at three, six, nine or 12 months.
Opioid use, both short-term and long-term, is associated with a high rate of multiple adverse effects. More than 500,000 Americans have died by overdosing on prescription opioids since 2000.1 Moreover, long-acting opioids are associated with a 90 percent increased risk for all-cause mortality compared with control medications.7 The risk of death increases more than 400 percent in the first 30 days of treatment with opioids.
Interestingly, other medications are not better options than opioids. According to a systematic review published in Annals of Internal Medicine, researchers found little to no benefit for NSAIDs, antidepressants, muscle relaxants, acetaminophen or anticonvulsants in patients with chronic low back pain.2
Rethinking Chronic Pain With Pain Neuroscience Education
In the past 20 years, we have learned a lot about chronic pain. One non-pharmacological approach, called pain neuroscience education, has demonstrated some impressive patient outcomes.
 Pain neuroscience education is an educational strategy that focuses on teaching patients in pain how to change their beliefs regarding their pain. It consists of educational sessions explaining the neurobiology and neurophysiology of pain, and how pain is processed by the nervous system.
Pain neuroscience education is an educational strategy that focuses on teaching patients in pain how to change their beliefs regarding their pain. It consists of educational sessions explaining the neurobiology and neurophysiology of pain, and how pain is processed by the nervous system.
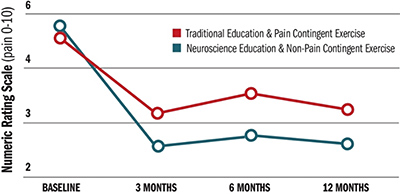
Malfliet and colleagues conducted a multi-center, randomized, clinical trial to compare pain neuroscience education and non-pain-contingent exercise with general education and pain-contingent exercise in individuals with chronic spinal pain (> 3 months).6 This study was published in JAMA Neurology.
Participants in the experimental group received pain neuroscience education and non-pain-contingent exercise (patients performed an exercise 10 times, regardless of the pain). Participants in the control group received traditional back and neck education, and pain-contingent exercise therapy (when participants reported pain during or after an exercise, the intensity or duration of the exercise was reduced).
Both groups experienced reduced pain at three, six and 12 months, but the pain neuroscience education and non-pain-contingent exercise group had greater improvements at all three follow-ups. This experimental group also experienced improved function and better mental health compared to controls at all three time points.
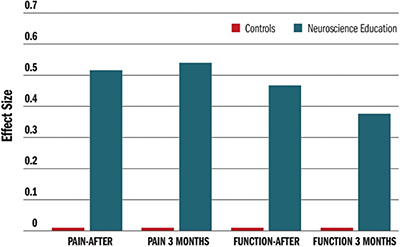
Tegner, et al., conducted a systematic review and meta-analysis to evaluate the effect of pain neuroscience education for patients with chronic low back pain.9 They systematically searched six databases and included seven randomized, controlled trials in their review. The pain neuroscience education group had reduced pain intensity and lower disability immediately after treatment and three months later, but the control groups did not.
The statistic "effect size" was used to demonsrtate treatment benefit. The larger the effect size, the larger the benefit. Pain neuroscience education combined with non-pain-contingent exercise training is effective in reducing pain, improving function and improving mental health in patients with serious chronic spinal pain. Adding pain neuroscience education with non-pain-contingent exercise to our current therapeutic package of care will offer considerable benefit to patients with chronic pain.
A Chiropractic Program on Pain Neuroscience Education
Over the past several years, a pain neuroscience education program designed for chiropractic clinics has produced dramatic patient outcomes.3 A typical patient in this population has had chronic pain for more than two years and has taken medication (usually opioids) without a significant reduction in pain. However, after pain neuroscience education, the average patient's pain is reduced by 54.2 percent.
References
- Burke DS. Forecasting the opioid epidemic. Science, 2016;354(6312):529.
- Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults - United States, 2016. MMWR Morb Mortal Wkly Rep, 2018;67:1001-1006.
- Chou R, Deyo R, Friedly J, et al. Systemic Pharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med, 2017;166:480-492.
- Feise RJ. Pain Neuroscience education and Non-Pain-Contingent Rehab Program. Institute of Evidence-Based Chiropractic, Scottsdale, Ariz., 2018.
- Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011.
- Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs. nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: The SPACE Randomized Clinical Trial. JAMA, 2018;319:872-882.
- Malfliet A, Kregel J, Coppieters I, et al. Effect of pain neuroscience education combined with cognition-targeted motor control training on chronic spinal pain: a randomized clinical trial. JAMA Neurol, 2018;75:808-817.
- Ray WA, Chung CP, Murray KT, et al. Prescription of long-acting opioids and mortality in patients with chronic noncancer pain. JAMA, 2016;315:2415-23.
- Reuben DB, Alvanzo AA, Ashikaga T, et al. National Institutes of Health Pathways to Prevention Workshop: the role of opioids in the treatment of chronic pain. Ann Intern Med, 2015;162(4):295-300.
- Tegner H, Frederiksen P, Esbensen BA, Juhl C. Neurophysiological pain education for patients with chronic low back pain: a systematic review and meta-analysis. Clin J Pain, 2018;34:778-786.
- Vowles KE, McEntee ML, Julnes PS, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain, 2015;156(4):569-576.
Click here for more information about Ronald Feise, DC.





