I can't remember how many lumbar films I've read and just reported, "atherosclerotic plaquing of the abdominal aorta," leaving it at that. My only concern was to rule out aneurysmal enlargement. I don't generally mention anything in my impressions regarding atherosclerosis involving the abdominal aorta unless there is an enlargement of ≥ 3 cm. I just assume the patient is aware they have cardiovascular disease.
I'm sure many of you discuss this with patients, but possibly not often enough. Prevention is the key. It should start with lifestyle modification including weight management, nutrition and physical activity. Of course, smoking cessation everyone should know. The American Heart Association's "Life's Simple 7: Avoiding Heart Failure and Preserving Cardiac Structure and Function" offers extremely helpful patient management tools.1
Radiological Indicators
We should be playing a more prominent role in primary care when it comes to heart disease. Our patients often come to us for musculoskeletal disorders, primarily back pain.2-3 Cardiovascular disease can present clinically as back pain. We also know degenerative disc disease has a vascular component.4
Calcification in the abdominal aorta detected on lateral lumbar radiographs is an indicator of subclinical atherosclerotic disease, and a predictor of subsequent vascular disease elsewhere in the body. This is a common finding on plain films; it can be extremely useful in predicting the extent of cardiovascular disease, and is used as an important predictor of vascular morbidity and mortality.
What percentage of your patients have presented with low back pain as the primary complaint? At least 80 percent probably have lumbar spine films from your office or some other source.
The AAC-24 Score
An easy tool you can use to evaluate the extent of cardiovascular disease is the Abdominal Aortic Calcification (AAC)-24. The Framingham Heart Study created this simple, inexpensive tool to assess the severity of calcific plaque formation in the abdominal aorta.6
Here's how it works: On a lateral lumbar film, trace the aorta from L1 through L4, both the anterior and posterior margins. Score the amount of calcification as follows:
- 0: no aortic calcific deposits
- 1: small scattered calcific deposits filling less than one-third of the longitudinal wall of the aorta
- 2: one-third or more, but less than two-thirds of the longitudinal wall of the aorta calcified
- 3: two-thirds or more of the longitudinal wall of the aorta calcified
These scores are tallied for each vertebral level L1-L4; both at the anterior and posterior wall of the aorta. Add up the number from at all levels including anterior and posterior; that is the score. Sounds crude and simple, but it is inexpensive and works well. Minimum score is 0 and maximum is 24.7 The AAC-24 score actually also correlates well with carotid artery atherosclerosis.8 The higher the score, the higher the incidence of cardiovascular disease elsewhere.
The Significance of AAC
Abdominal aortic calcification (AAC) is a marker of subclinical atherosclerotic disease, and an independent predictor of subsequent vascular morbidity and mortality. Not only is it an indicator of hypertension and hyperlipidemia; it is also associated with carotid artery plaque, spine degeneration, chronic kidney disease, even loss of bone mass and increased hip and vertebral body fracture.
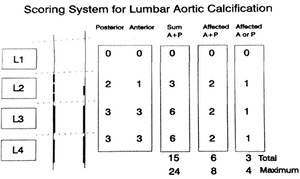 FIG 1 ACC-24 scoring system from the Framington Heart Study.
Vascular, bone and joint diseases are chronic age-related diseases that share many common dietary and lifestyle risk factors, and cause considerable morbidity and mortality. In the past, the consensus held that these diseases were not related. More recent literature and research has proven there is a strong link between osteoporosis and cardiovascular disease. Additionally, the underlying processes regulating arterial calcification share many similarities to bone physiology and systemic bone homeostasis.
FIG 1 ACC-24 scoring system from the Framington Heart Study.
Vascular, bone and joint diseases are chronic age-related diseases that share many common dietary and lifestyle risk factors, and cause considerable morbidity and mortality. In the past, the consensus held that these diseases were not related. More recent literature and research has proven there is a strong link between osteoporosis and cardiovascular disease. Additionally, the underlying processes regulating arterial calcification share many similarities to bone physiology and systemic bone homeostasis.
AAC is also independently associated with cardiovascular events in dialysis patients and in the general population. Now, even with non-dialysis chronic kidney disease (CKD) patients, the extent of abdominal aortic calcification can be used to identify CKD patients at higher cardiovascular risk and may provide important information for personalized treatment.
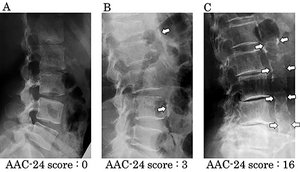 FIG 2 ACC-24 score determined on weight-bearing lateral lumbar film.
Atherosclerotic calcific plaquing in the abdominal aorta generally begins around the major vessel bifurcations and branching arteries, such as the inferior mesenteric artery and the lumbar arteries. Occlusion of these vessels causes ischemia to the blood supply to the lumbar vertebrae and intervertebral discs, resulting in disc degeneration, facet degeneration and asymptomatic vertebral fractures. Assessment of lateral spine images aids in the detection of vertebral fractures and has been shown to improve fracture prediction.9-11
FIG 2 ACC-24 score determined on weight-bearing lateral lumbar film.
Atherosclerotic calcific plaquing in the abdominal aorta generally begins around the major vessel bifurcations and branching arteries, such as the inferior mesenteric artery and the lumbar arteries. Occlusion of these vessels causes ischemia to the blood supply to the lumbar vertebrae and intervertebral discs, resulting in disc degeneration, facet degeneration and asymptomatic vertebral fractures. Assessment of lateral spine images aids in the detection of vertebral fractures and has been shown to improve fracture prediction.9-11
The regulation of arterial calcification is physiologically similar to the regulation of the osseous skeleton. The calcified atherosclerotic plaques release both local and systemic osteochondrogenic factors that may affect regional and systemic bone homeostasis.5 Conversely, circulating levels of factors regulating bone homeostasis may also regulate vascular calcifications,6 with a number of studies demonstrating osteoporosis and low bone mineral density (BMD) as risk factors for cardiovascular disease (CVD).7-8
A high AAC score indicates the whole body is suffering from vascular disease; some organs are affected sooner that others. It means it is time to make some drastic lifestyle changes.
Our Opportunity and Responsibility
Approximately 15.4 million Americans ages 20 years or older have coronary heart disease (CHD). Asymptomatic disease is even more prevalent. The sad truth is that CHD is mostly preventable. This year, 2020, CHD is estimated to become the leading cause of death and disability worldwide.
Despite this high prevalence, atherosclerosis can be greatly slowed and its consequences markedly reduced by preventive measures. Prevention means making healthy lifestyle choices to prevent the development of coronary risk factors; or at the very least delaying or preventing the onset of clinically symptomatic cardiovascular disease.
Chiropractors have been on the forefront of teaching their patients lifestyle changes with musculoskeletal alignment, nutrition, exercise, etc. We need to continue to encourage our patients to adopt a healthier lifestyle. Prevention is the goal; lifestyle modification is the treatment.
References
- Mok Y, Sang Y, Ballew SH, et al. American Heart Association's Life's Simple 7 at Middle Age and Prognosis After Myocardial Infarction in Later Life. J Am Heart Assoc, 2018;7(4):e007658.
- Suri P, et al. Vascular disease is associated with facet joint osteoarthritis. Osteoarthr Cartilage, 2010 ;18(9):1127-1132.
- Beckworth WJ, et al. Atherosclerotic Disease and its Relationship to Lumbar Degenerative Disk Disease, Facet Arthritis, and Stenosis with Computed Tomography Angiography. PM&R, 2018;10(4):331-337.
- Kauppila LI, McAlindon T, Evans S, et al. Disc degeneration/back pain and calcification of the abdominal aorta. A 25-year follow-up study in Framingham. Spine, 1997;22:1642-1647.
- Wilson PW, Kauppila LI, O'Donnell CJ, et al. Abdominal aortic calcific deposits are an important predictor of vascular morbidity and mortality. Circulation, 2001;103(11):1529-1534.
- Kauppila LI, et al. New indices to classify location, severity, and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis, 1997 Jul;132(1997):245-250.
- Kobayashi K, et al. Carotid artery plaque screening using abdominal aortic calcification on lumbar radiographs. PLoS One, 2019;14(1):e0209175.
- Friedlander AH, et al. Detection of carotid artery calcification on the panoramic images of post-menopausal females is significantly associated with severe abdominal aortic calcification: a risk indicator of future adverse vascular events. Dento Maxillo Facial Radiol, 2015;44(7):20150094.
- RodrÃguez AJ, Leow K, Szulc P, et al. Abdominal aortic calcification, bone mineral density and fractures: a systematic review and meta-analysis protocol. BMJ Open, 2019;9(4):e026232.
- Farhat GN, Cauley JA. The link between osteoporosis and cardiovascular disease. Clin Cases Miner Bone Metab, 2008;5(1):19-34.
- Thompson B, Towler DA. Arterial calcification and bone physiology: role of the bone-vascular axis. Nat Rev Endocrinol, 2012;8(9):529-543.
- Szulc P. Abdominal aortic calcification: a reappraisal of epidemiological and pathophysiological data. Bone, 2016; 84:25-37.
- Peeters MJ, et al. Abdominal aortic calcification in patients with CKD. J Nephrol, 2017;30(1):109-118.
- Lillemark L, et al. Growth patterns of abdominal atherosclerotic calcified deposits from lumbar lateral X-rays. Int J Cardiovasc Imaging, 2010;26(7):751-761.
- Suri P, et al., Op Cit.
- Go AS, Mozaffarian D, Roger VL, et al., for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics - 2014 update: a report from the American Heart Association. Circulation, 2014 Jan 21;129(3):e28-e292.
- Strasser T. Reflections on cardiovascular diseases. Interdisciplinary Sci Rev, 1978;3:225-30.
- Eckel RH, Jakicic JM, Ard JD, et al., for the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation, 2014 Jun 24;129(25 suppl 2):S76-99.
Click here for more information about Deborah Pate, DC, DACBR.





