Osteoarthritis of the hip affects more than 4 million people in the U.S., and over 200,000 primary elective total hip replacements (THR) are performed per year.
| Indications for THR Revision According to the Swedish Hip Arthroplasty Register |
|
| Reason for Revision | Rate of Occurrence |
| Aseptic Loosening | 75% |
| Deep Joint Infection | 8% |
| Dislocation | 6% |
| Fracture | 5% |
| Technical Error | 3% |
| Implant Fracture | 1% |
| Other | 4% |
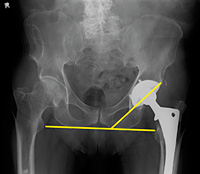 Figure 1: Angle of inclination 40o +/- 10°.
Of course, as chiropractors we are not able to do anything about these complications, but we should evaluate any patient with a THR who has symptoms that might indicate problems with the THR. A simple AP pelvis view can be very helpful in determining if there are problems with the THR. If the patient has their initial baseline X-rays, a quick comparison can be employed to evaluate even slight changes in the prosthesis. Alignment and positioning should mimic normal anatomy.
Figure 1: Angle of inclination 40o +/- 10°.
Of course, as chiropractors we are not able to do anything about these complications, but we should evaluate any patient with a THR who has symptoms that might indicate problems with the THR. A simple AP pelvis view can be very helpful in determining if there are problems with the THR. If the patient has their initial baseline X-rays, a quick comparison can be employed to evaluate even slight changes in the prosthesis. Alignment and positioning should mimic normal anatomy.
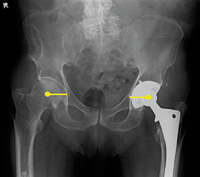 Figure 2: Center of rotation should be equal for both hips.
The position of the acetabular component and the stem can be easily assessed on an AP view. The acetabular angle of inclination should be 40 degrees +/- 10 degrees. (Figure 1) Anteversion cannot be assessed on the AP and a frog leg view is very difficult to obtain in these patients, so CT is often used to assess this angle. The center of rotation, however, can be assessed on the AP view. (Figure 2)
Figure 2: Center of rotation should be equal for both hips.
The position of the acetabular component and the stem can be easily assessed on an AP view. The acetabular angle of inclination should be 40 degrees +/- 10 degrees. (Figure 1) Anteversion cannot be assessed on the AP and a frog leg view is very difficult to obtain in these patients, so CT is often used to assess this angle. The center of rotation, however, can be assessed on the AP view. (Figure 2)
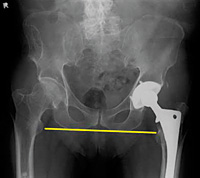 Figure 3: Leg-length discrepancy measured by comparing the lesser trochanter position (they should be parallel).
The distance from center of the femoral head to teardrop (or other identifiable landmark) should be equal bilaterally. The iliopsoas tendon should pass just lateral to the center of the femoral head and helps to keep the hip in proper alignment. Excessive lateral positioning of the acetabular component results in the iliopsoas tendon crossing medial to the femoral head, placing the patient at risk for dislocation.
Figure 3: Leg-length discrepancy measured by comparing the lesser trochanter position (they should be parallel).
The distance from center of the femoral head to teardrop (or other identifiable landmark) should be equal bilaterally. The iliopsoas tendon should pass just lateral to the center of the femoral head and helps to keep the hip in proper alignment. Excessive lateral positioning of the acetabular component results in the iliopsoas tendon crossing medial to the femoral head, placing the patient at risk for dislocation.
 Figure 4: Loosening of the stem of the femoral component of the THR.
The center of the rotation will be different when comparing the hips. Leg-length discrepancy can also be a factor in THR complications. (Figure 3) This can also be assessed on the AP projection. The only other view one needs to take is an AP view of the THR side (which includes the femoral stem) to rule out loosening of the stem. (Figure 4)
Figure 4: Loosening of the stem of the femoral component of the THR.
The center of the rotation will be different when comparing the hips. Leg-length discrepancy can also be a factor in THR complications. (Figure 3) This can also be assessed on the AP projection. The only other view one needs to take is an AP view of the THR side (which includes the femoral stem) to rule out loosening of the stem. (Figure 4)
These are just basis assessments of a THR, but will help in determining if the patient's symptoms are attributable to a problem with the THR. Most patients do well with total hip replacements, but when problems develop, chiropractors may be the first to see the patient. These simple assessments will help determine if the patient needs further follow-up and revision.
Click here for more information about Deborah Pate, DC, DACBR.





