Many of my patients (and probably many of yours) come in with pain and/or tenderness in the buttock region. First, I assess where the painful and/or tender spots are located and what these points represent. The answer is not simple; many points have overlap. I do a quick treatment (ideally a self-treatment) to verify my diagnostic hypothesis. As usual, I use tenderness as a reality check. My goal is to markedly reduce the tenderness via some combination of exercise, manipulation and/or soft-tissue work.
1. Assess for Lumbar (Axial) Discogenic Pain
Is lumbar disc pain frequent? Authorities estimate 40-50 percent of patients who see a doctor for lower back pain have an underlying disc problem.1 These percentages are consistent with my clinical experience ... once I understood how to assess for this condition.
My impression is that chiropractors, PTs and osteopaths tend to miss this condition, and overdiagnose SI and lower lumbar facet problems. Discogenic sciatica is easier to diagnose. Axial discogenic pain has a different history and exam presentation. Read my articles2 and/or look at the work of Stuart McGill, PhD (www.backfitpro.com) and Phillip Snell, DC (www.fixyourownback.com and its clinical companion class).
Lumbar disc pain usually expresses as some combination of midline, central achy pain, with some buttock referral. The pain is often hard for the patient to localize. The buttock pain will usually be close to the midline, over the sacrum or just lateral and inferior to it. (Note that this tender area has a huge overlap with sacrotuberous ligament origin, piriformis origin and/or sacroiliac pain referral zones.)
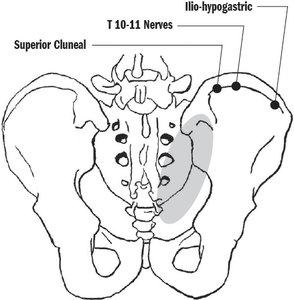 Black circles represent tender nerve points in Maigne's syndrome; gray oval represents referral zones in axial disc pain.
Here is a simple test: With the patient prone, find the tender buttock spot. Ask the patient to rate pain severity. Then have them do three 20-second repeats of McKenzie extension. Does the tender point disappear or diminish? If it has, then my disc diagnosis is confirmed, and the patient now has a pain-relieving exercise to do on their own.
Black circles represent tender nerve points in Maigne's syndrome; gray oval represents referral zones in axial disc pain.
Here is a simple test: With the patient prone, find the tender buttock spot. Ask the patient to rate pain severity. Then have them do three 20-second repeats of McKenzie extension. Does the tender point disappear or diminish? If it has, then my disc diagnosis is confirmed, and the patient now has a pain-relieving exercise to do on their own.
2. Maigne's Syndrome: Cluneal Nerve Pain With Thoracolumbar Dysfunction
Maigne's is common and significant, despite being rarely diagnosed. Learn the cluneal nerve anatomy. The main tender nerve points are more lateral than the disc referral. They are found just below the iliac crest, starting 7-8 cm lateral to the midline and going out to the mid-axillary line. This condition is usually unilateral.3
It's a simple exam: 1) With the patient prone or sitting, explore the area just below the iliac crest. The specific tender spots will feel nodular and swollen. The patient can tell you this is their pain, or they can be surprised by these tender points. 2) Assess the spine, from L3 up to T10. Look for tenderness either over the facets or on the involved side of the spinous processes.
The global treatment is to adjust the spine; the local treatment is to treat the nerve all along its pathway. I prefer YAP / DTM,4 wiggling and lifting the superficial fascia and the nerve. If this diminishes the tenderness, I instruct the patient on how to do this frequently at home.
3. Assess the Hip for Tender Points, Especially Around the Hip
Hip dysfunction can directly cause hip or buttock pain. The pain can be on the lateral side of the hip, or in the groin, anterior hip or occasionally posterior hip area.
I see lots of back and buttock pain in which the hips contribute to lower back pain, but are not the direct cause of the pain. This is part of the joint-by-joint hypothesis. When the hip lacks proper motion, the lower back has to move too much. This will affect vulnerable lumbar discs, lumbar facets and/or the sacroiliac.
I find a lack of normal motion, especially internal rotation, accompanied by tenderness over the head of the femur. These are the two major indicators of functional hip impingement, which means the patient's femur is not seated properly in the acetabulum.5
I differ from most rehab approaches here. This is not just a lack of mobility of the hip; it is a specific pattern, with the femur is stuck forward. The best correction involves combining the right mobilization with specific exercises that re-center the hip back into its socket. The patient has to stop trying to open their hip!6
4. Neurologically Inhibited Gluteal Muscles Secondary to UC Fixation
Here's one I have not shared much, but have found extremely valuable. Virtually the whole buttock is covered by the glutes. Assess for weakness on manual muscle testing of the gluteus maximus and/or gluteus medius. If either is weak, further assess the upper cervical spine for spinal fixation. Recheck strength and tender points after adjusting. The entire extensor chain can be reflexively inhibited by upper cervical dysfunction.
According to applied kinesiology, when there is weakness of the bilateral gluteus maximus, it means there is an upper cervical fixation (a complex of three vertebrae stuck). I'm not an AK doc, but this pattern has helped me with numerous challenging cases.
I've observed that the weak muscle could be either the gluteus maximus or gluteus medius. Sometimes the patient will have bilateral weakness; sometimes unilateral weakness. In any of these cases, check the upper cervical. Sometimes I find a three-vertebra fixation; sometimes I just find unilateral dysfunction.
Consider a case involving a 70-year-old female with years of right buttock pain. She was disabled and depressed by frequent episodes of deep buttock severe "spasms." My first five treatments did not do much. Tried disc, hip and Maigne approaches without success.
She said, "What about my piriformis? That is where the pain is." The piriformis was very tender at both its origin and its insertion. (You have to side lie the patient to properly assess the insertion of the piriformis.) Direct soft tissue did not do much. I finally muscle tested and found her right gluteus maximus was weak. That led to the upper cervical; I found fixation and adjusted it.
She had immediate strengthening of her gluteus maximus. The piriformis immediately relaxed. She recovered, and finally had her life back.
Note: Don't forget rehab. You are seeing the neurology immediately change. The muscle has not worked properly for months to years. The patient needs rehab to restore actual strength and endurance. You need to be both the magician and the coach.
5. Short Leg: Assess Weight-Bearing
Sometimes a heel lift is the ideal global treatment to provide in this situation.
6. Buttock Pain Originally (Mis)diagnosed as Sacroiliac Pain
Although I have become an SI skeptic, sacroiliac pain and SI dysfunction referral do exist. Unless the patient has three or more positive provocation tests, I'll start with correcting the other factors above and then re-assess SI alignment.
Author's Note: In my next article, I will go into more detail on local treatments to specific tender buttock points.
References
- Michael A, et al. Biomechanics of Back Pain. Churchill Livingstone, 2012.
- Heller M, Snell P. "Flexion Intolerant Lower Back Pain, Part One: Diagnosis." Dynamic Chiropractic, Jan. 15, 2014.
- Heller M. "How to Find and Fix TL Nerve Impingements." Dynamic Chiropractic, April 15, 2016.
- Heller M. "More Solutions for TL Fixations & Nerve Irritation." Dynamic Chiropractic, Nov. 1, 2017.
- Heller M. "Functional Hip Impingement, Part 1." Dynamic Chiropractic, April 15, 2015.
- Heller M. "Functional Hip Impingement, Part 2: Rehab Exercises." Dynamic Chiropractic, May 1, 2015.
Click here for more information about Marc Heller, DC.





