"Carpal Tunnel" will be seen in this column often because of the extent of the emphasis on it today. What follows would be a very conservative and thorough medical investigation as to the diagnosis of carpal tunnel. This will allow better to discuss alternative treatment regimens with company medical personnel in order to initiate preventive concepts.
- Hyperesthesia or paresthesia in the median nerve distribution (tingling, pain, and numbness). This is never in the fifth finger on close questioning. Usually worse during rest after work.
- Weakness of the thumb with grasping or pinching.
- Symptoms occasionally improve with shaking or rubbing the hands.
Characteristics of the Syndrome
- More common in women.
- More common in the working (30-50) age group.
- Much more common in the right, or dominant hand.
- Both hands involved one-half of the time.
- Symptoms often after work, at night.
- Often described as poor circulation.
- Often described as involving the whole hand (fifth finger is really not).
- Pain often referred to the forearm or arm.
Physical Findings
- Hypersthesia of the median nerve distribution (80%). Use sterile or alcohol clean needle for examination or light touch.
- Atrophy of thenar muscles (late).
- Weakness of five-finger pinch with thumb.
- Tinel's sign (70%) - paresthesia with digital percussion (tapping) directly on the median nerve.
- Phalen's sign (70%) - paresthesia produced by two minutes of maximal flexion of the wrist joint.
- Increased pain or paresthesia with arm blood pressure cuff over systolic blood pressure one to two minutes.
- EMG usually reveals increased conduction delay (latency).
- Primarily, CTS is a clinical diagnosis. The EMG is occasionally normal with CTS and may be abnormal in employees without symptoms.
Differential Diagnosis
Pathology proximal to the wrist may cause pain in the hand; CTS may cause referred pain to the forearm and elbow. This causes uncertainty at times and prompts more extensive examination to rule out cervical causes (disc, arthritis, etc.) Scalenicus anticus syndrome or cervical rib (Adson test) as well as thoracic outlet syndrome, and vascular problems (Allen test) must be considered. Tendinitis, epicondylitis, neuropathies and psychosomatic disorders, as well as malingering, are other uncommon conditions in the differential diagnosis.
Electromyography
The time of condition of an electric impulse (85 millivolts) from one point of a nerve to another point can be measured and compared with the normal. The motor and sensory fibers are measured separately.
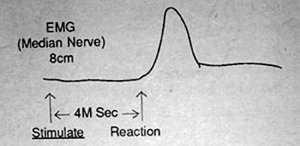 Pathology at the wrist is detected by placing an electrode on the wrist over the distal flexion crease directly over the median nerve and a second electrode over the abductor pollicis longus (thenar eminence). They are exactly eight cm apart. The time between stimulation of the proximal electrode and the muscle contraction is measured. This motor conduction time is normally less than four milliseconds.
Pathology at the wrist is detected by placing an electrode on the wrist over the distal flexion crease directly over the median nerve and a second electrode over the abductor pollicis longus (thenar eminence). They are exactly eight cm apart. The time between stimulation of the proximal electrode and the muscle contraction is measured. This motor conduction time is normally less than four milliseconds.
The hand electrode is placed over a sensory area without motor function, and the interval from stimulation to reception again is measured (a nerve conducts in either direction). The sensory conduction of 8 cm is not over 3 milliseconds (one millisecond faster than a motor conduction). When the conduction time (latency) is prolonged, the nerve function between the two points is impaired.
The examiner, then, in a similar manner measures the nerve function from the biceps to the proximal wrist to establish the function of a nerve elsewhere for comparison.
Click here for previous articles by Theodore Oslay, DC.





