The prevalence of pregnancy-related low back pain and disability is significant. According to a review of the literature, the mean prevalence of pregnancy-related low back pain is about half of all pregnancies.1-2 Most women report a return to pre-pregnancy levels of low back pain within six months of delivery, but some go on to experience chronic low back pain. Research reports a postpartum prevalence of 37 percent at one year and 18 percent at six years.3
There are two main approaches to the management of chronic pelvic pain – pharmacological or non-pharmacological. Let's take a look at the effectiveness and safety of each approach.
The Pharmacological Approach
Horne, et al., conducteda randomized, double-blind, placebo-controlled trial to measure the efficacy and safety of gabapentin in women with chronic pelvic pain.5 More than 300 participants were randomly assigned to receive gabapentin or a placebo for 16 weeks.
 Treatment with gabapentin compared with placebo did not result in lower pain scores in women with chronic pelvic pain, and it was associated with higher rates of side effects than placebo.
Treatment with gabapentin compared with placebo did not result in lower pain scores in women with chronic pelvic pain, and it was associated with higher rates of side effects than placebo.
Although acetaminophen and NSAIDs offer a modest amount of pain relief, they have a poor safety profile. Maternal acetaminophen use during pregnancy is associated with a higher risk for attention-deficit disorder and autism spectrum disorder in children.6 Additionally, two meta-analyses found an association between the use of acetaminophen during pregnancy and asthma in children.7-8
Increased risks of miscarriage and malformations are associated with NSAID use in early pregnancy.9 Exposure to NSAIDs after 30 weeks' gestation is associated with an increased risk of premature closure of the fetal ductus.10 Li, et al., demonstrated that NSAID use around conception was associated with an increased risk of miscarriage with a dose-response relationship.11
Non-Pharmacological Approach
An effective non-pharmacological approach to pelvic pain includes an individualized treatment program consisting of: 1) adequately informing and reassuring the patient, 2) individualized exercises, and 3) spinal manipulation.
Exercises: An individualized exercise program that includes stabilizing exercises and aerobic exercise is part of an effective treatment strategy for pregnant patients with back or pelvic pain. In a randomized, controlled trial, researchers found that stabilizing exercises had a significantly better statistical and clinical effect than the controls on pain, functional status and health-related quality of life measured after 20 weeks of intervention and one year postpartum.12 A Cochrane systematic review confirmed these findings.13
Aerobic exercise contributes to the overall treatment plan for patients with spinal pain, because it is associated with improvements in mood state and overall feeling of well-being, strengthening the supporting spinal musculature, improving neuromotor control and coordination, and increasing nutrition for the disc. Thus, current research supports an exercise program of strengthening exercises and aerobic exercise.
Spinal Manipulation: Researchers have found that spinal manipulation can provide safe and effective relief of back and pelvic pain in pregnant women. A randomized clinical trial examined the effects of a chiropractic multimodal approach (including stabilization exercises) compared to standard obstetric care.14 The research team was composed of medical doctors and chiropractors, and the findings were published in the American Journal of Obstetrics & Gynecology.
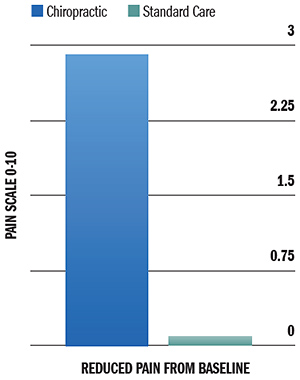
The graph titled "Improvements in Pain" demonstrates the conclusions of this study. This graph shows the effect size of treatments for pain. "Effect size" is a measure of treatment benefit. The larger the effect size, the better the result. The chiropractic approach demonstrated clinically important reductions in pain compared with standard obstetric care.
Moreover, multiple systematic reviews support the conclusion that chiropractic treatment is a safe and effective intervention for reducing pain intensity and frequency in pregnant women with back and pelvic pain.15-16
Science Supports Conservative Care
Chiropractic care is the premier non-pharmacological choice for patients with chronic pelvic pain. We need to communicate the safety and effectiveness of our approach not only to our patients, but also to medical doctors and insurance companies. You can build your practice by sharing this information with OB-GYN doctors, paying close attention to what you say and even more attention to what not to say to them.
References
- Ansari NN. Low back pain during pregnancy in Iranian women: prevalence and risk factors. Physiother Theory Pract, 2010;26:40-8.
- Mogren IM, Pohjanen AI. Low back pain and pelvic pain during pregnancy: prevalence and risk factors. Spine, 2005;30:983-91.
- Stapleton DB, et al The prevalence of recalled low back pain during and after pregnancy: a South Australian population survey. Aust N Z J Obstet Gynaecol, 2002;42:482-5.
- MacEvilly M, Buggy D. Back pain and pregnancy: a review. Pain, 1996;64:405-14.
- Horne A, et al. Gabapentin for chronic pelvic pain in women (GaPP2): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet, 2020;396:909-917.
- Ji Y, et al. Association of cord plasma biomarkers of in utero acetaminophen exposure with risk of attention-deficit/hyperactivity disorder and autism spectrum disorder in childhood. JAMA Psychiatry, 2019 Oct 30:1-11.
- Eyers S, et al. Paracetamol in pregnancy and the risk of wheezing in offspring: a systematic review and meta-analysis. Clin Exp Allergy, 2011;41:482-9.
- Etminan M, et al. Acetaminophen use and the risk of asthma in children and adults: a systematic review and meta-analysis. Chest, 2009;136:1316-23.
- Edwards DR, et al. Periconceptional over-the-counter nonsteroidal anti-inflammatory drug exposure and risk for spontaneous abortion. Obstet Gynecol, 2012;120:113-22.
- Musu M, et al. Acute nephrotoxicity of NSAID from the foetus to the adult. Eur Rev Med Pharmacol Sci, 2011;15:1461-72.
- Li DK, et al. Use of NSAIDs during pregnancy and the risk of miscarriage. Am J Obstet Gynecol, 2018;219:275.e1-275.
- Stuge B, et al. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy. A randomized controlled trial. Spine, 2004;29:351-359.
- Pennick VE, Young G. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev, 2007;(2):CD001139.
- George JW, et al. A randomized controlled trial comparing a multimodal intervention and standard obstetrics care for low back and pelvic pain in pregnancy. Am J Obstet Gynecol, 2013;208:295.e1-7.
- Khorsan R, et al. Manipulative therapy for pregnancy and related conditions: a systematic review. Obstet Gynecol Surv, 2009;64:416-27.
- Stuber KJ, Smith DL. Chiropractic treatment of pregnancy-related low back pain: a systematic review of the evidence. J Manipulative Physiol Ther, 2008;31:447-54.
Author's Note: The research presented in this article is also available in video format at https://chiroevidence.com/research-capsule-240.
Click here for more information about Ronald Feise, DC.





