Temporomandibular joint (TMJ) syndrome can be one of the most difficult and elusive conditions to treat.
Patients can suffer with symptoms, despite years of traditional medical therapy.
One of the primary reasons for a poor outcome in TMJ treatment is a lack of clinical understanding of the relationship between articular, muscular and neurological causes of the condition. If any of these potential causative factors are missing in the treatment approach, poor results can occur. The doctor who diagnoses and treats all factors will notice an increase in positive results and patient satisfaction.
TMJ Anatomy
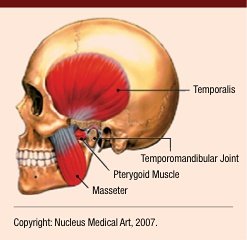
The temporomandibular joint is the articulation between the condyle of the mandible and the squamous portion of the temporal bone. An internal disk known as the meniscus is a fibrous, saddle-shaped structure that separates the condyle and the temporal bone. The meniscus and its attachments divide the joint into superior and inferior spaces.1 These disks not only act to separate the hard bones, but also to absorb and cushion vibrations and impact transmitted through the joint.
The TMJ is controlled by muscles. The muscles controlling the TMJ are predominantly the masticatory muscles including the temporalis, masseter, lateral pterygoid, medial pterygoid and buccinator. However, other muscles may have an effect on the functioning of the TMJ such as the neck, shoulder and back muscles.2 This is the key area overlooked by physicians when treating TMJ syndrome. Primary muscles include the scalene, sternocleidomastoid, trapezius, levator scapulae, supraspinatus, infraspinatus, rhomboids and latissimus dorsi. There has even been a case in which the soleus muscle affected the TMJ via kinetic-chain dysfunction.
 Causes: Arthritis is one cause of TMJ symptoms. It can result from an injury or from grinding the teeth at night. Another common cause involves displacement or dislocation of the disk that is located between the jawbone and the socket. A displaced disk may produce clicking or popping sounds, limit jaw movement and cause pain when opening and closing the mouth.
Causes: Arthritis is one cause of TMJ symptoms. It can result from an injury or from grinding the teeth at night. Another common cause involves displacement or dislocation of the disk that is located between the jawbone and the socket. A displaced disk may produce clicking or popping sounds, limit jaw movement and cause pain when opening and closing the mouth.
The disk also can develop a hole or perforation, which can produce a grating sound with joint movement.3 Bruxism (teeth grinding) causes micro-trauma to the joint capsule, ligaments and soft tissue, leading to symptoms from active trigger points and adhesions.
Common symptoms: Clicking or popping, bruxism, headaches, earaches, dizziness, eye pain and neck/shoulder pain.
Integrative Treatment
One must take into consideration all of the physiological and anatomical structures listed above. Starting with a three-day-a-week program, the following therapy approach has proven to be successful in alleviating symptoms associated with TMJ dysfunction.
Laser Therapy
The bio-stimulation, anti-inflammation, and pain-alleviating effects of laser light are what makes this therapy so special and of prime importance. Laser dosages of between 600 and 700 joules per side are recommended. Be sure to aim the laser inside the joint capsule with the jaw open and cover all the trigger points found on palpation. You may also laser the pterygoid muscles from inside the mouth.
If TMJ symptoms are due to arthritis, laser therapy may be the only therapeutic modality to offer lasting pain relief. Due to treatment time constraints and penetration capabilities of low-level cold lasers, higher-power class-4 therapy lasers may be the preferred instrument of choice.
Trigger Points
Check all of the muscles previously listed. You may use ART, MRT, TPT or MFR depending on your skill level. Primary trigger points include the pterygoids, sternocleidomastoid, scalene and temporalis. These points can be excruciatingly painful when treated, so make sure to prepare the patient. Active trigger points may take six to 10 therapy sessions for resolution. If you feel comfortable, do trigger-point therapy with a gloved finger to the pterygoids inside the mouth.
Check the infraspinatus carefully. These points are typically latent and only present pain on palpation. A knotted infraspinatus causes internal rotation of the glenohumeral joint and external rotation of the scapulae, leading to over-recruitment of the rhomboids and trapezius, resulting in forward-head carriage. This abnormal posture over-stimulates the scalene and sternocleidomastoid muscles, causing faulty TMJ mechanics and an elevated first rib.
Check the latissimus dorsi attachment at the thoracolumbar junction. Myofascial adhesions here can restrict normal scapular motion during glenohumeral abduction, resulting in cervical kyphosis and altered righting mechanisms via kinetic-chain dysfunction. MFR and ART can be very successful in this region. A high dose of laser therapy along the entire thoracolumbar region with a dosage of 1,000 joules can break up chronic adhesions that have been lying dormant for years. This can be the "magic bullet" area for unresolved shoulder and neck disorders, too. Don't overlook it!
Articular
Check for a hypomobile occiput and atlas articulation. I have found occiput is the primary culprit, usually subluxated posterior. An elevated first rib may cause a kinetic-chain alteration with the sternoclavicular joint, resulting in overactive neck flexors. Normalizing a subluxated first rib can have an immediate pain-relieving effect on TMJ pain and chronic trapezius muscle spasm. Speed is of utmost importance when adjusting a first rib.
I only recommend manually adjusting a TMJ if you have specialized training in TMJ disorders or if you work directly with a TMJ specialist. Adjusting the wrong side, an incorrect line of drive or a hypermobile joint can have severe pain-inducing consequences.
Cranial
Using a gloved finger/thumb, put superior pressure for five seconds on the center of the hard palate and then bilaterally on the horizontal plate by the back molars. Repeat three times while the patient inhales slowly, releasing pressure as the patient exhales. This technique normalizes function of the sphenoid bone, which can improve TMJ mechanics.
As you can see, success in TMJ treatment involves looking way outside of the proverbial box. The word integrate means "to make something part of a larger whole, or be joined or made part of a larger whole." Remember to look at the whole patient and don't get caught up in the vicious cycle of targeted symptomatic care. This integrated treatment protocol can give profound improvement to your patients' quality of life. Take the time to implement them; your patients will be glad you did, and so will you.
References
- Basmajian J. Muscles Alive. Baltimore: Williams and Wilkins, 1974.
- III Gillespie T. TMJ Anatomy. Accessed Oct. 12, 2007 from University of Washington: www.rad.washington.edu/anatomy/modules/ TMJ/TMJAnatomy.html.
- NYU Medical Center. Accessed Oct. 11, 2007, from www.med.nyu.edu/surgery/oral/patients/ article.html.
Click here for more information about Perry Nickelston, DC, FMS, SFMA.





