Probably no area of clinical practice is more confusing to chiropractic patients than the subject of short leg. Even among the chiropractic profession, there are differing opinions regarding this phenomenon.
Practitioners who commonly utilize the "Derifield-Thompson" test of comparing heel lengths with a patient prone often do not explain to their patients that any appearance of leg-length inequality using this method is usually functional - a result of muscle imbalance, rather than a true difference in the length of the long bones. Those who use this test to confirm or dispel the rebalancing of the spine and pelvis give credence to its validity, although most studies have found little reliability or reproducibility using the exam.
The whole process has always been somewhat of a mystery to me. My instructor at Palmer could not explain the mechanism, and the only possible way I know to explain the appearance of change in heel height with a patient prone and knees flexed is as a difference in quadriceps tonus.
Anatomical leg-length inequality (LLI) is a very different matter. Often overlooked on initial examination and unappreciated, LLI can have a significant effect on the pelvis and spine from both an anatomical and biomechanical perspective.
 The advantage of open-back gowning for all new patients is that one can make a comprehensive structural and postural visual exam with a patient erect, beginning with the feet and ankles and working up. Ignoring this essential first step in examination has resulted in many overlooked factors to chronic pelvic and spinal pain. I have patients disrobe to their underwear and ask female patients to remove their bra for an unobstructed view of the spine.
The advantage of open-back gowning for all new patients is that one can make a comprehensive structural and postural visual exam with a patient erect, beginning with the feet and ankles and working up. Ignoring this essential first step in examination has resulted in many overlooked factors to chronic pelvic and spinal pain. I have patients disrobe to their underwear and ask female patients to remove their bra for an unobstructed view of the spine.
One telling sign of possible anatomical leg-length inequality is declination to one side of the underwear or panty line that follows the inferior tilt of the sacrum and pelvis. Another consistent sign of LLI is asymmetry of the flank fat fold. Also, one commonly sees an elevated shoulder on the side of the anatomically short leg, a result of compensatory rotoscoliosis. Palpating the crest of the ilia simultaneously will often reveal pelvic imbalance, as it appears pelvic torsion and obliquity almost always accompanies LLI. As a method to help confirm the probability of anatomical short leg, I place the patient supine on a flat table with shoes on. I then have them draw their knees to their chest, roll into a ball, and then carefully extend lumbar, pelvis and lower extremities, eventually lying flat with the feet slightly off the table. With my thumbs on the bottom of the patient's shoes, under the arch, pressing lightly cephalid, I can assess any appearance of true LLI by viewing heel discrepancy.
Measurements for LLI using a tape measure and various landmasses have proven quite unreliable, showing no consistency of findings or even the ability to correctly identify the side of the short leg. I consider visual and palpatory signs of a short leg while erect, combined with a confirming supine leg-length test, to be justification for X-ray to validate the impression and make measurements for possible lift therapy.
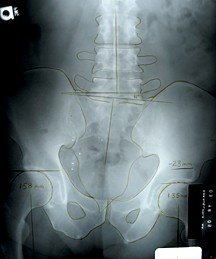
It seems universally accepted that the only accurate measurement for LLI is an erect A-P pelvic X-ray with center beam through the top of the femur heads. Great care should be taken in proper patient placement and posture. Once in position, I instruct a patient to fully extend both knees, bring them forward equally to a point of comfort, and then hold. One also should be aware of the effect unilateral hyperpronation of the ankle and foot may have on leg-length measurement. To compensate for such a development, I instruct the patient to roll both feet outward and then slowly lower them until both feet are properly balanced with a vertical Achilles' tendon. The X-ray tube should be absolutely perpendicular to the film with the center of the beam at the ilio-femoral joint space, hitting the middle of the film.
Once a good image has been secured, measuring from the bottom of the film to a horizontal line drawn at the top of the femur heads will give a comparative difference indicating true leg-length inequality.
One also may measure a line at the sacral base against horizontal for the angle of sacral base declination. For those wishing to identify which of the lower extremity long bones is short or in what combination, one may use the same technique to get an A-P bilateral knee view. I have even done this combined, using collimation for a split-screen view on 14"x17" film mounted vertically.
The next consideration is how much leg-length inequality is clinically significant and worthy of attention. With the incidence of some LLI being estimated to be very high among the general population (as much as 90 percent), many doctors have been taught that anything less than 1 inch (25 mm) LLI is not clinically significant and is within the body's adaptive capacity. This view was supported by studies identifying many asymptomatic patients with such differences in leg length. Although not generally accepted by the osteopathic or chiropractic professions, it is indicative of how much opinion can vary. Given the variable factors that can influence conscious pain perception, the reality of silent inflammation, capsulitis, paraspinal myospasm and articular dyskinesia in the presence of spinal biomechanical impairment (chronic occult subluxation), one could reasonably question the absolute relevance of studies that relate LLI to only conscious pain. Some studies have identified as much as 75 percent incidence of LLI in patients suffering chronic low back pain, and others state that even a few millimeters of asymmetry may constitute a primary or contributing cause for low back symptoms and advanced degenerative change in the lumbar spine. I use the 5 mm LLI minimum rule in practice and utilize lift therapy above this amount.
How much and how to lift a short leg is another age-old debate. While there can be differences of opinion on this subject, a few constants seem worth noting. It is generally accepted that the upper limit of simple heel-lift therapy using in-shoe wedged pads is 10 mm, or about 3/8 inch. Lifting above this amount with a wedge device is not recommend, so as to not adversely effect alignment and biomechanics of knee function or shorten the Achilles' tendon. Beyond this limit, it is recommended that a patient employ a full sole/external heel lift combination. Another constant is that if LLI is a result of trauma, as from a fracture of the tibia or femur, then it is generally safe to lift the full amount of measured inequality - provided there has not been an excessive time period (decades) walking in adaptive compensation. Finally, all agree that lift therapy should be done in stages, with some time given for adaptation between elevations.
The "golden rule" of lift therapy for developmental LLI used by many early practitioners of physical medicine was to lift to one-half of the measured leg-length inequality. The reasoning is that various adaptive compensations may have developed during maturation, such as vertebral body wedging and muscle and connective tissue density change. In recognition of these necessary and permanent adaptations, by lifting to only one half of the measured LLI, one chooses to work with the adaptive changes rather than against them, stopping short of full correction. Of course, a very young patient may be somewhat the exception to this rule. Also, with femur and tibia growth rates being dependent on shifting load patterns as one matures - one side catching up to the other in growth spurts - premature lift therapy below the age of skeletal ossification generally is not advisable.
To identify LLI and other structural/postural abnormalities by first making a comprehensive visual examination is the duty of all who specialize in neuromusculoskeletal disorders. Correctly measuring through X-ray and then addressing LLI by lift therapy relieves chronic postural stressors and decreases the probability of degenerative lumbar spinal change over a lifetime. Additionally, when applied correctly, heel-lift therapy may help greatly in reducing chronic low back pain.
Dr. John Bomar, a 1978 graduate of Palmer College of Chiropractic, practices in Arkadelphia, Ark. He is a past board member of the Arkansas Chiropractic Association and a founding board member of the Arkansas Chiropractic Educational Society. Contact Dr. Bomar with questions and/or comments regarding this article via e-mail:
.




