When one treats whiplash-injured patients, occasionally chiropractic testimony will become necessary. Treating chiropractors testify as experts for the plaintiff (injured patient). Insurance defense attorneys usually attempt to minimize (challenge, discredit, refute, embarrass, etc.) the importance and relevance of the plaintiff chiropractor's testimony.
The Case in Question
In a recent case of uncontested injury and liability, the defense essentially conceded these classic chiropractor testimony issues:
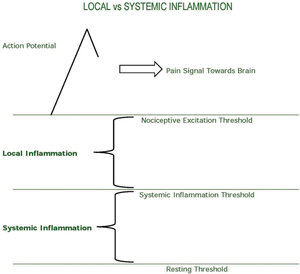
- Injury causes local inflammation.
- Local inflammation alters the nociceptive afferent threshold (causes pain).
- Resolution of inflammation is fibrosis.
- Fibrosis reduces injured joint movement parameters and alters the instantaneous axis of rotation (creating the orthopedic component of the subluxation complex).
- Reduced and/or altered joint movement parameters proportionally reduce mechanical afferentation (proprioception) toward the central neural axis, rendering the pain gate chronically open and resulting in chronic pain.
- Applied, specific line-of-drive mechanical forces (chiropractic adjustment) would realign the developing fibrosis tissue along the direction of the applied forces, improving joint movement parameters, improving mechanoreception (proprioception), closing the pain gate, and reducing pain perception.
- This line of reasoning and evidence is supported by history, complaint, examination, imaging (especially stress radiography), and standard functional measurement outcome assessments.
The Defense's Argument
 So, where did the defense go during the cross-examination of the treating chiropractic expert? They went to issues pertaining to systemic inflammation (as contrasted to local inflammation) as impacting the magnitude of the patient's pain, the duration of the patient's pain, the recovery of pain and function, and the residuals documented on functional measurement outcomes. Their basic argument was this:
So, where did the defense go during the cross-examination of the treating chiropractic expert? They went to issues pertaining to systemic inflammation (as contrasted to local inflammation) as impacting the magnitude of the patient's pain, the duration of the patient's pain, the recovery of pain and function, and the residuals documented on functional measurement outcomes. Their basic argument was this:
Total Inflammation = Local Inflammation + Systemic Inflammation
Their argument (simplified) was that the patient's pain and disability are established by the patient's total inflammation. Yet, the injury caused only the local inflammatory component of the patient's total inflammation. Therefore, they argued that any component of the patient's clinical status attributed to systemic inflammation was not their responsibility.
This argument is weak, as attorneys often state that all injured people get equal protection under the law, including the frail (including those with pre-injury systemic inflammation). Hence, they used an extension of the argument by claiming that the standard of care in chiropractic is to treat not only the local inflammation, but also the systemic inflammatory issues in order to optimize recovery rates, and reduce residual pain and functional problems.
Nutritional Supplementation and the Standard of Care
The attorney was well-educated, articulate and very knowledgeable about a number of related systemic inflammatory variables. These included diet (consumption of alcohol, refined carbohydrates, red meat, etc.), exercise, sleep hygiene, antioxidant supplements, and more.
His primary line of questioning centered around the ratio of omega-6 to omega-3 fatty acids. His eloquent argument was that the standard of care for chiropractors was to assess and recommend omega-3 fatty acid supplementation for all patients in pain, including those injured in a whiplash accident. His argument included:
- If the treating chiropractor does not assess the omega-6 to omega-3 ratio and intervene appropriately, the chiropractor is practicing below the standard of care. As such, any nociceptive and/or functional residuals are ascribed to substandard chiropractic care and not to the injuries sustained in the accident.
- If the patient does not follow the advice of the treating chiropractor in reducing his systemic inflammatory profile (like taking omega-3 supplements), any nociceptive and/or functional residuals are ascribed to the patient and not to the injuries sustained in the accident.
This attorney was obviously very well-versed and prepared with information for his argument. Ironically, after all the years of discounting the role supplementation can play in the recovery of an injured patient by this P.I. industry and insurance companies, he actually argued to validate nutritional efficacy while representing an insurance company.
I advocate assessing the omega-6:omega-3 ratio in all patients (I do). It is a quick, simple fingerprick analysis that is very informative. The most anti-inflammatory component of fish oil is eicosapentaenoic acid (EPA); as such, I prefer a formula that has a higher level of EPA, preferably a ratio of 2:1 of EPA:DHA (DHA = docosahexaenoic acid).
Classically, dosing is determined by the labs, but in general, supplementation is not likely to achieve an anti-inflammatory profile without consuming 3,000 mg daily of EPA + DHA (EPA 2,000 mg; DHA 1,000 mg).
There are other interesting factors that warrant review and discussion, but I'll leave that for another time.
Resources
- Stoll A. Omega-3 Connection. Simon & Schuster, 2001.
- Sears B. The Omega Zone. Regan Books, 2002.
- Sears B. The Anti-Inflammation Zone. Regan Books, 2005.
- Boswell M, Cole BE (editors). Weiner's Pain Management; A Practical Guide for Clinicians, 7th Edition. American Academy of Pain Management, 2006.
- Maroon JC, Bost JW. Omega-3 fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain. Surg Neurol, April 2006;65:326-331.
- Cleland LG, James MJ, Proudman SM. Fish oil: what the prescriber needs to know. Arthritis Res & Ther, 2006;8(1):402.
- Goldberg RJ, Katz J. A meta-analysis of the analgesic effects of omega-3 polyunsaturated fatty acid supplementation for inflammatory joint pain. Pain, May 2007;129(1-2):210-223.
- Simopoulos AP. Evolutionary aspects of diet: the omega-6/omega-3 ratio and the brain. Molec Neurobiol, October 2011;44;(2):203-215.
- Davis W. Wheat Belly Total Health. Rodale Books, 2014.
Dr. Dan Murphy is a 1978 graduate of Western States Chiropractic College (now the University of Western States) and diplomate of the American Board of Chiropractic Orthopedics. He has taught more than 1,500 continuing-education classes on various topics including clinical nutrition, biomechanics, soft-tissue injury and repair, and the management of spine and spine-related conditions; and is a contributing author on several books, including Motor Vehicle Collision Injuries and Pediatric Chiropractic.