Sometime in the early 1980s, I read a book called Low Back and Leg Pain from Herniated Cervical Disc1 by Herman Kabat, who was also the developer of proprioceptive neuromuscular facilitation (PNF) stretching.
All of that was interesting enough, but what really piqued my interest was the manual examination method Kabat described to detect these cervical disc herniations. He found that the patient with occult cervical disc pathology would exhibit a weakness of the wrist flexor muscle, the adductor pollicis muscle, and the peroneal muscles, all on the side of the body corresponding to the herniated nucleus pulposus. He further found that the weakness of these muscles could be temporarily abolished by mild and temporary distraction of the cervical spine, and exacerbated by mild and temporary cervical compression.
Naturally, this all seemed very much drawn out of applied kinesiology (AK), a technique I was greatly interested in around 1985. In Kabat's work, we had what might be described as a previously strong or weak indicator muscle changing its strength as such and such was "challenged." As a chiropractor, I wasn't that interested in Kabat's treatment program for these patients (patients whom I now say satisfy "Kabat's criteria"), which involved self-administered traction and avoiding certain movements and activities that he believed would put stress on the herniated disc. On the other hand, I was fascinated with the concept that herniated cervical discs could mimic herniated lumbar discs, and so, I set about using the methods of AK to determine what manipulative approach and line of drive would constitute the best approach to the problem.
Using the vertebral challenge, as described by Walther,2 I found (much to my surprise) that I needed to adjust patients satisfying Kabat's criteria using an anterior to posterior line of drive in the lower cervical spine, and on the side of muscle weakness. I didn't really know how to do that, but I found that I could modify the traditional modified rotary break to get the job done. The setup for adjusting "anterior cervical syndrome," as I started calling this subluxation, is identical to that of the modified rotary break (MRB), except that the tissue pull and thrust have a slight A to P component. I call the adjustment the "anterior cervical break." Figure 1 portrays the move, but a still photo does not do it justice and does not distinguish it from the more conventional MRB.
Although my personal interest in using AK had waned by the end of the 1980s, I did continue to follow the work. One of my students took an AK seminar from David Leaf, and came home with printed seminar notes describing "hidden cervical disc." Amazingly, practitioners of AK, presumably using challenge methods similar, if not identical, to those I had used, had come to a similar mechanical conclusion. On the other hand, maybe it isn't that amazing that examiners using the same method came to the same conclusions. In addition, I have been told that Dr. Stonebrink, technique maven at Western States Chiropractic College, developed an analysis and correction of an anterior cervical subluxation, and that the Motion Palpation Institute also teaches an anterior cervical adjustment.
Sure enough, I also found this anterior cervical syndrome in the writings of Walther,3 whom I regard as the most coherent writer in the AK community. In preparing this article, I noticed at his Web site that the International College of Applied Kinesiology Board of Standards has decided to change the name of the "hidden cervical disc" to "anterior cervical subluxation." I have used the term "anterior cervical syndrome," including in my office patient charts, for many years.
Using static and motion palpation to further characterize patients with Kabat's criteria, I ultimately came to the conclusion that they tended to exhibit fixation on the side of muscle weakness, as well as spinous process rotation toward that same side of fixation. (Of course, such a conclusion was self-serving: having decided on the basis of a vertebral challenge that I need to thrust from A to P, it was very convenient for me to decide that the spinous process had rotated toward the side of contact.) Anyway, I ultimately concluded that Kabat's patients had spinous process rotation toward the side of fixation.
Pursuing the mechanical logic a bit further, let us see what happens in a diversified technique setting to a patient who exhibits fixation in the lower cervical spine on the side of spinous process rotation. The classic diversified strategy of performing an MRB opposite the side of spinous process rotation won't do, because that is not the fixated side. However, neither will apply an MRB on the fixated side, because that would make the rotational misalignment worse. The obvious solution, however unconventional the line of drive, would be a thrust on the side of fixation, with an anterior to posterior component to the vector.
Thus, there are at least two ways of getting to the anterior cervical break adjustment: the patient satisfies Kabat's criteria; or the patient has spinous process rotation toward the side of lower cervical fixation. I really don't know if these two patient populations are the same, overlap, or if one is a subset of the other. In figure 2a, the patient populations overlap, but some who lack Kabat's criteria may exhibit the characteristic palpatory findings, and vice versa. In figure 2b, the set of Kabat's patients includes a smaller subset with the palpatory findings; and in figure 2c, the set of patients with the palpatory finding includes the smaller set of those satisfying Kabat's criteria.
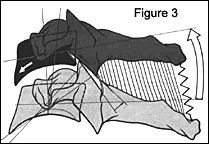
In the anterior cervical break, the contact point on the patient is on the anterior aspect of the transverse process on the involved side. Although this may seem odd to some, especially those chiropractors who believe a vertebra can only subluxate posteriorly in relation to the segment below, anterior subluxation obviously occurs. Figure 3 (modified from Kapandji),4 depicts anterior cervical subluxation, a fixation within a position that occurs during forward flexion of the neck, in which anterior flexion is coupled to anterior glide of the segment above.
In my implementation, the doctor uses an A to P tissue pull, with the head and neck flexed toward and rotated away from the contact hand, just like the setup for the conventional modified rotary break. The suggested ratio for the line of drive is 90 percent lateral to medial, and 10 percent anterior to posterior; a more dramatic A to P vector makes the adjustment too difficult to perform, and is also unnecessary. Students and other inexperienced adjusters are cautioned against attempting this move before having mastered the modified rotary break and the lateral break, in that order, as it is relatively difficult to perform. A lateral break, such as that described by Bergmann and Zachman,5 may be somewhat less optimal, but will be effective enough and more comfortable for the patient until this anterior adjustment is mastered.
For some reason, I sometimes fail to accomplish the anterior cervical break on the right side, although I rarely miss it on the left. I do not know if this reflects something about me as an adjustor, or a property of my patients, having to do with handedness or some other consideration.
References
- Kabat H. Low Back and Leg Pain from Herniated Cervical Disc. St. Louis, Missouri: Warren H. Green, Inc.; 1980.
- Walther DS. Applied Kinesiology, Volume I. Pueblo, Colorado: Systems DC; 1981.
- Walther DS. Applied Kinesiology: Synopsis. Pueblo, Colorado: Systems DC; 1988.
- Kapandji A. The Physiology of the Joints, Volume 3. Edinburgh London and New York: Churchill Livingstone; 1974.
- Bergmann TF, Zachman ZJ. An approach to specific correction of lateral flexion joint dysfunction. Chir Tech 1989;1(2):46-51.
Dr. Robert Cooperstein, a professor at Palmer College of Chiropractic West, can be reached at www.chiroaccess.com, or by e-mail at
.
Click here for previous articles by Robert Cooperstein, MA, DC.