Your patient's medical doctor recommended skeletal muscle relaxants for his acute low back pain, but the patient does not want to take medication. He is a delivery person who had a bad reaction to skeletal muscle relaxants in the past. How should you respond to your patient's concerns? What does the current research say?
Muscle Relaxants vs. Manipulations
Today we compare the benefits of muscle relaxants with those of chiropractic manipulations. A randomized, double-blind clinical trial has tested the efficacy of chiropractic manipulation, muscle relaxants and placebo for subacute low back pain.2 This study was published in the Journal of Manipulative and Physiological Therapeutics. The research team consisted of four chiropractors, two PhDs and one MD.
 More than 190 patients experiencing low back pain of 2-6 weeks' duration were randomly allocated to three intervention groups: chiropractic manipulations with placebo medicine, muscle relaxants with sham manipulations, or placebo medicine with sham manipulations.
More than 190 patients experiencing low back pain of 2-6 weeks' duration were randomly allocated to three intervention groups: chiropractic manipulations with placebo medicine, muscle relaxants with sham manipulations, or placebo medicine with sham manipulations.
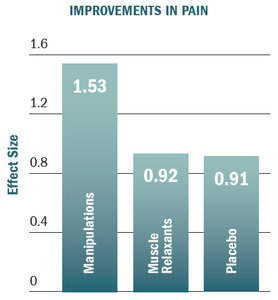
The bar graph titled, "Improvements in Pain" demonstrates this study's conclusions. This graph shows the effect size of treatments for pain. "Effect size" is a measure of treatment benefit. The larger the effect size, the better the result.
Chiropractic manipulations were 49 percent more effective than muscle relaxants or placebo for reducing pain. Note that muscle relaxants were not even better than placebo. These findings hold true at different measurement times and also apply to patient function.
Additional Research on Muscle Relaxants for Acute Low Back Pain
The early clinical trials for muscle relaxants found modest improvements in pain and function, but these studies were of poor quality. In 1988, a randomized, clinical trial found muscle relaxants had no effects superior to placebo.3 Then in 2011, another research team found different results. In a pharmaceutical industry-led clinical trial, researches found a 24 percent improvement in pain with muscle relaxants compared to placebo.4 (It is important to note that these findings have never been duplicated.)
Recently, a research team conducted a systematic review and meta-analysis to investigate whether including unpublished quality randomized, clinical trial data changed the benefits for patients with low back pain. They found that the addition of unpublished quality data reduced the benefit of muscle relaxants for acute low back pain. The benefit, originally published as 22 percent improvement, was reduced to 2 percent when that data was added.5
Another research team conducted a prospective analysis of four quality randomized, placebo-controlled studies to determine the effects of seven popular skeletal muscle relaxants (baclofen, metaxalone, tizanidine, diazepam, orphenadrine, methocarbamol, and cyclobenzaprine) in patients with acute low back pain.6 This research team discovered that patients with acute LBP who are treated with these skeletal muscle relaxants do not experience outcomes better than placebo.
In light of the latest research, there is currently a lack of evidence to support the use of muscle relaxants for acute low back pain.
Muscle Relaxants for Chronic Low Back Pain or Sciatica
The U.S. Department of Health and Human Services sponsored a systematic review that investigated the effects of muscle relaxants on patients with chronic low back pain.7 The research team found no evidence that muscle relaxants were consistently better than placebo. Additionally, there is no research demonstrating benefits of muscle relaxants for patients with sciatica.
Not Just Ineffective – Dangerous
Numerous adverse reactions are associated with muscle relaxants. In particular, skeletal muscle relaxants are associated with heart failure, paralysis, difficulty breathing, tachycardia, chest pain, sudden numbness or weakness, sudden headache, confusion, fainting, weakness, lack of coordination, hallucinations and problems with vision, speech, or balance.
Multiple clinical trials have found that skeletal muscle relaxants are associated with 50 percent more total adverse events and 104 percent more central nervous system adverse events than placebo.8 In a nationwide case-control study of Medicare patients, the use of skeletal muscle relaxants was associated with a 40 percent increase in fracture risk.9
Since 2004, there has been an 84 percent increase in skeletal muscle relaxant involvement in suicide attempts.10 Furthermore, among patients who were already taking muscle relaxants at the time of their doctor visit, 67.2 percent were concomitantly treated with an opioid – a combination known to cause serious drug-drug interactions and an increased risk of opioid overdose.1
Based on the lack of evidence regarding the long-term safety of muscle relaxants and their risk of abuse, guideline recommendations limit the use of these drugs to a maximum duration of 1-2 weeks.1 Despite these recommendations, a study found that 44.5 percent of people taking muscle relaxants were continuously treated with these drugs for longer than one year.11
Our Opportunity
The results of this research present an opportunity. Medical doctors and their patients will be searching for effective and safe alternatives. Evidence-based chiropractors will be welcomed. Additionally, insurance companies should notify patients and medical providers that they will no longer pay for muscle relaxants, because they are ineffective and unsafe for back pain.
Author's Note: The research presented in this article is also available in video format at https://chiroevidence.com/research-capsule-240/.
References
- Soprano SE, Hennessy S, Bilker WB, Leonard CE. Assessment of Physician Prescribing of Muscle Relaxants in the United States, 2005-2016. JAMA Netw Open 2020;3:e207664.
- Hoiriis KT, Pfleger B, McDuffie FC, Cotsonis G, Elsangak O, Hinson R, Verzosa GT. A randomized clinical trial comparing chiropractic adjustments to muscle relaxants for subacute low back pain. J Manipulative Physiol Ther 2004;27:388-98.
- Berry H, Hutchinson DR. A Multicentre Placebo-Controlled Study in General Practice to Evaluate the Efficacy and Safety of Tizanidine in Acute Low-Back Pain. Journal of International Medical Research 1988:75-82.
- Chandanwale, A.S., Chopra, A., Goregaonkar, A., Medhi, B., Shah, V., Gaikwad, S., Langade, D.G., Maroli, S., Mehta, S.C., Naikwadi, A., Pawar, D.R. (2011). Evaluation of eperisone hydrochloride in the treatment of acute musculoskeletal spasm associated with low back pain: A randomized, double-blind, placebo-controlled trial. J Postgrad Med 2011;57:278–285.
- Bagg MK, O'Hagan E, Zahara P, Wand BM, Hubscher M, Moseley GL, McAuley JH. Systematic reviews that include only published data may overestimate the effectiveness of analgesic medicines for low back pain: a systematic review and meta-analysis. J Clin Epidemiol 2020;124:149-159.
- Abril L, Friedman B. The Efficacy of Skeletal Muscle Relaxants in Emergency Department Patients With Low Back Pain. Albert Einstein College of Medicine. American College of Emergency Physicians (ACEP) 2020: Abstract 15. 2020.
- Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, Fu R, Dana T, Kraegel P, Griffin J, Grusing S, Brodt E. Noninvasive Treatments for Low Back Pain. Comparative Effectiveness Review No. 169. AHRQ Publication No. 16-EHC004- EF. Rockville, MD: Agency for Healthcare Research and Quality; February 2016.
- van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM. Muscle relaxants for non-specific low back pain. Cochrane Database Syst Rev. 2003: CD004252.
- Witenko C, Moorman-Li R, Motycka C, et al. Considerations for the appropriate use of skeletal muscle relaxants for the management of acute low back pain. P & T : a peer-reviewed journal for formulary management. 2014;39(6):427-435.
- Substance Abuse and Mental Health Services Administration, DrugAbuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits. HHS Publication No. (SMA) 13-4760, DAWN Series D-39. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2013.
- Dillon C, Paulose-Ram R, Hirsch R, Gu Q. Skeletal muscle relaxant use in the united states: Data from the third National Health and Nutrition Examination Survey (NHANES III). Spine (Phila Pa 1976) 2004;29:892-896.
Click here for more information about Ronald Feise, DC.





