The hip joint is an absolutely critical component of both lower back and lower extremity problems. I want to share what I have learned recently. First, it's important to note a couple of studies that confirm the importance of the hip.
Addressing the hip joint is important in many cases, not just patients who complain of hip or groin pain. In another fascinating study,3 a clinical prediction rule, therapists looked at which patients would respond most consistently to a simple lumbar manipulation. They found that one of the significant factors was normal hip internal rotation. Think outside the box and reverse this. It implies that in the tougher cases, those that need more comprehensive care, patients lack normal hip internal rotation.
Let's look at the hip joint and how to address it. Over the years, I have noticed two very common subluxation patterns in the hip. The first is a lack of internal rotation. This fits the Cyriax capsular pattern, in which internal rotation is the first motion lost in hip joint problems. When you find a severe lack of internal rotation in the hip and this motion cannot be restored, the patient is usually on their way to hip replacement surgery, sooner or later. If you can restore near-normal motion, the hip-related pain usually will improve, and hip surgery can be avoided or at least delayed. In my clinical experience, I have found this lack of internal rotation to be clinically significant and very helpful in establishing a prognosis.
 The second subluxation pattern seen is a lack of anterior-to-posterior motion, and what you might call an anterior hip. I'm not usually a fan of muscle-testing indicators (where weakness "A" means dysfunction "B"), but I make an exception in certain cases. Lucy Whyte Ferguson, in a chapter on the hip in her book Clinical Mastery in the Treatment of Myofascial Pain,4 describes weakness of the hip flexors, including the psoas, rectus femoris or TFL, indicating that the hip joint is dysfunctional. I was taught this many years ago,5 and it's one of the findings that has stood the test of time in my own practice.
The second subluxation pattern seen is a lack of anterior-to-posterior motion, and what you might call an anterior hip. I'm not usually a fan of muscle-testing indicators (where weakness "A" means dysfunction "B"), but I make an exception in certain cases. Lucy Whyte Ferguson, in a chapter on the hip in her book Clinical Mastery in the Treatment of Myofascial Pain,4 describes weakness of the hip flexors, including the psoas, rectus femoris or TFL, indicating that the hip joint is dysfunctional. I was taught this many years ago,5 and it's one of the findings that has stood the test of time in my own practice.
Over the years, I have looked for these two subluxation patterns and corrected them,6 and seen good changes in my patients. Then I read Dr. Whyte Ferguson's chapter on the disordered hip complex and the whole picture suddenly became much clearer. Dr. Whyte Ferguson puts the whole thing together. She talks about these two joint patterns and sees them as one - a combination of positional external rotation and anterior subluxation that leaves the head of femur on the anterolateral edge of the acetabulum, not fully "seated." I'll describe how to correct this later in the article.
Myofascial Components of Hip Pain
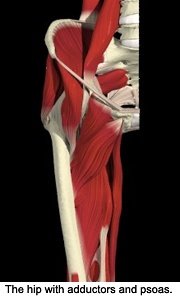
The myofascial component is critical to correcting the dysfunctional hip. Before reading Dr. Whyte Ferguson's work, my focus was on the obvious tight muscles behind the trochanter. This includes the gluteal insertions, the piriformis and other external rotators. There are other critical muscles. Dr. Whyte Ferguson outlines what she calls the "bowstring" and "rubber band" metaphors; how the hypertonic psoas and adductors pull the head of the femur out of position.
 If you understand the biomechanics of the bowstring metaphor, it will change how you look at the hip forever. Think about the psoas and the adductors. Both frequently are tight, and both have significant myofascial shortening. The psoas inserts at the lesser trochanter. When it is tight, it pulls the femur in an anterolateral direction. This is reinforced by the adductors, which are pulling the shaft of the femur in a medial direction. The combination of these two pulls shifts the femur in its socket, leaving the femoral head stuck more anterior and more lateral than it belongs. This model makes so much sense clinically.
If you understand the biomechanics of the bowstring metaphor, it will change how you look at the hip forever. Think about the psoas and the adductors. Both frequently are tight, and both have significant myofascial shortening. The psoas inserts at the lesser trochanter. When it is tight, it pulls the femur in an anterolateral direction. This is reinforced by the adductors, which are pulling the shaft of the femur in a medial direction. The combination of these two pulls shifts the femur in its socket, leaving the femoral head stuck more anterior and more lateral than it belongs. This model makes so much sense clinically.
What muscles should you assess and release? As mentioned, key muscles include the adductors, the psoas and iliacus, the gluteus medius and maximus, as well as the piriformis, quadratus femoris and the other small external rotators of the hip. Don't forget the TFL and the iliotibial band. Dr. Whyte Ferguson introduces a different way to evaluate trigger points and tight bands. Instead of evaluating while the muscle is at rest, she moderately stretches the muscle, and then palpates for tight bands. You are not taking the muscle to a fully stretched position, just a partial stretch. When I first tried this on the adductors, it was like a light- bulb went off. You'll find many more trigger points and tight bands.
What does the patient need to do? First, avoid any exercises (such as a sitting adductor stretch) that take the hip into external rotation, at least until the hip joint is stable. Second, the patient needs to learn to use their hip and buttock muscles properly. This is beyond the scope of this article, but think of a proper hip hinge in getting up and down from sitting, and look at the spine length squat in my article on pain-relief exercise.7 The spine length squat emphasizes firing the core while internally rotating the hips, and pushing the buttock posterior to emphasize the lumbar curve.
Adjusting the Hip
 Dr. Whyte Ferguson describes an elegant adjustment using eccentric contraction of the adductors to help the practitioner guide the hip back into a properly seated position, simultaneously correcting both the anterior and the external rotation parts of the subluxation pattern. She calls it the "wishbone maneuver." In this manipulation, you take the hip from near-neutral into flexion, abduction and internal rotation, while the patient resists your action by eccentrically activating their adductors.
Dr. Whyte Ferguson describes an elegant adjustment using eccentric contraction of the adductors to help the practitioner guide the hip back into a properly seated position, simultaneously correcting both the anterior and the external rotation parts of the subluxation pattern. She calls it the "wishbone maneuver." In this manipulation, you take the hip from near-neutral into flexion, abduction and internal rotation, while the patient resists your action by eccentrically activating their adductors.
The patient is lying supine, with the legs hip-width apart. The following example will address the right hip. The clinician starts off facing perpendicular to the table. With your active right arm, cradle the patient's bent knee, supporting the leg both above and below the knee. Begin to lift the whole leg into slight flexion, slight abduction and slight internal rotation. Your other hand holds the left leg down on the table. (I have modified this maneuver, as I don't like to bend over - I just leave the other leg on the table.) You instruct the patient to use their muscles to pull the right knee toward the left knee. Find the verbal cue, knee to knee, or leg to thigh, that works best for the patient. Ask them to continue to do this as you move the leg. Take the whole leg smoothly into further flexion (ending between 90-110 degrees), abduction of 30 degrees and as much internal rotation as you can create without excessive force or stress. You end up facing toward the patient's feet.
You can retest to see if your adjustment was successful via changes in tenderness over the anterior femur, increases in internal rotation, and immediate changes in strength of the hip flexors. I have been very pleased with the profound changes in motion and end-feel that this adjustment creates. Addressing the hip joint and its surrounding musculature seems to have a lasting effect.
 This adjustment is unique. It will take you a few cases to get competent. It really is different to move a large limb while the patient continually pulls in the opposite direction. You need the patient's cooperation, coaching them to provide the "just right" amount of correction while you move the hip. It is not exactly muscle energy and it's not contract-relax; it's an eccentric long-lasting contraction during your mobilization. By having the patient actively contract all the way through the motion, the eccentric action of the adductors helps reset the joint. I suspect activation of the patient's internal rotators strongly inhibits the tight posterior hip muscles.
This adjustment is unique. It will take you a few cases to get competent. It really is different to move a large limb while the patient continually pulls in the opposite direction. You need the patient's cooperation, coaching them to provide the "just right" amount of correction while you move the hip. It is not exactly muscle energy and it's not contract-relax; it's an eccentric long-lasting contraction during your mobilization. By having the patient actively contract all the way through the motion, the eccentric action of the adductors helps reset the joint. I suspect activation of the patient's internal rotators strongly inhibits the tight posterior hip muscles.
Read Dr. Whyte Ferguson's recent article in the Journal of Bodywork and Movement Therapies,8 or better yet, the chapter on the hip in her book. Both of these describe these maneuvers and her overview of the disordered hip complex.
Low-force techniques have changed over the past 20 years. Chiropractors tend to think of the Activator or other adjusting instruments. You can integrate soft-tissue work with the adjustment. These techniques involve a more gradual motion that stretches the soft tissues as you move the joint. They involve some form of activation of the surrounding musculature, whether the contract-relax of muscle energy, the eccentric contraction with movement of the wishbone maneuver, the mobilization with movement of the Mulligan technique, instrument-assisted soft-tissue mobilization with provocation, or resistance and movement as taught in the third-level Graston technique class.
There is a theme here, and it goes something like this: Activate the whole neuromuscular axis as you treat. Re-educate the sensory and motor feedback loops as you adjust. Give the receptors, motor neurons and the whole neuraxis a completely different experience, so the body can reprogram its motion patterns.
References
- Goddard NJ, Gosling PT. Intra-articular fluid pressure and pain in osteoarthritis of the hip. J Bone Joint Surg Br, 1988;70:52-55.
- Imamura S, Riberto M, Fischer A, et al. Successful pain relief by treatment of myofascial components in patients with hip pathology scheduled for total hip replacement. J Musculokeletal Pain, 1998;6:73-89.
- Flynn T, et al. A clinical predictionrule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine, Dec. 15, 2002;27(24):2835-43.
- Whyte Ferguson L, Gerwin R. Clinical Mastery in the Treatment of Myofascial Pain. Lippincott, Williams & Wilkins, 2005.
- Thomas M. Lower extremity adjusting seminar, 1998; Eugene, Ore.
- Heller M. "The Hip Joint." Dynamic Chiropractic, Sept. 13, 2004. www.chiroweb.com/archives/22/19/15.html.
- Heller M. "Pain Relief Exercise: The Lower Back." Dynamic Chiropractic, Nov. 7, 2005. www.chiroweb.com/archives/23/23/11.html.
- Whyte Ferguson L. Knee Pain, Addressing the interrelationship between muscle and joint dysfunction in the hip and pelvis and the lower extremity. Journal of Bodywork and Movement Therapies, 2006;10:287-296.
Click here for more information about Marc Heller, DC.





