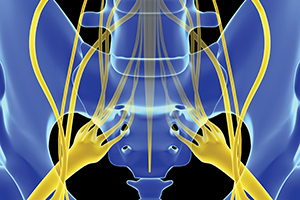
The thoracolumbar junction (TLJ) and the peripheral sensory nerves that exit from it are frequent, important and rarely recognized sources of lower back, pelvic and hip pain. Let's outline a clear exam protocol for diagnosing the problem.
I tend to be far too long-winded, so I am going to try to keep this short. If you are a geek like me and want more, go to my professional resources page on my website for my further thoughts on this topic,1 and read my previous articles on the TLJ and the upper lumbar by searching my online columnist page.
Exam for Spinal Dysfunction: T10 Through L3
Maigne used manual methods (and injections) to determine whether a specific vertebral segment was a significant source of pain. Maigne's protocol parallels Triano's rules. Triano, et al.,2 extensively reviewed the voluminous literature on the reliability of various tests manipulative therapists use. Quoting their work: "In general, the stronger and more favourable evidence is for those procedures which take a direct measure of the presumptive site of care – methods involving pain provocation upon palpation or localized tissue examination."
 Maigne described a concept of "painful minor vertebral dysfunction."3 (As a chiropractor, I might call the same thing a significant spinal fixation or subluxation.) Check out Maigne's paper on this. It is short and quite readable. I find myself agreeing with most of it. Here are the four steps he describes:
Maigne described a concept of "painful minor vertebral dysfunction."3 (As a chiropractor, I might call the same thing a significant spinal fixation or subluxation.) Check out Maigne's paper on this. It is short and quite readable. I find myself agreeing with most of it. Here are the four steps he describes:
- Pressure directly P-A on spinous process
- Transverse pressure against spinous process
- Longitudinal friction on facet joints
- Pressure on interspinous ligament
Let's apply this to the thoracolumbar junction. Start at T10 and work you way down to L3. (The only change I would add here: As you move lower into the mid-lumbar spine, you may find tenderness more effectively if you get below the involved facet joint and push it superior.) You'll note that most of these tests are extremely close to the midline. You are definitively on the vertebrae in question. Find the tender ones, estimate the spinal level and mark them with a skin pencil. I appreciate the simplicity of this exam protocol.
The spinal segment will probably show a lack of motion. Maigne is skeptical of our ability to palpate for motion deficits. I have been using motion palpation for 40 years and think it has enormous value. When I find a tender vertebra, I assess what directions it does not move freely in.
Palpating the Nerves
Why am I so interested in the thoracolumbar junction (and why should you be)? Most lower back and pelvic pain patients don't report pain in the TLJ. Maigne's hypothesis is that specific vertebrae in the region of the TLJ have painful minor vertebral dysfunction, and are a significant source of irritation to the peripheral sensory nerves that exit here. These nerves provide sensation to much of the flank, the lower back, and the pelvis and hips. When the nerves are irritated, the patient experiences pain. There is little research on this concept. It is further confused by the varying names researchers have given to this sensory nerve irritation.
What is pain? My pain science colleagues would probably differ with me here, but I would say pain comes primarily from irritated sensory nerves. Sensory nerves are designed to carry feedback back to the spinal cord and brain, telling us somewhere hurts.
Maigne has outlined simple protocols for this examination. We are looking for tenderness to palpatory pressure. In addition, you will feel what you could call swelling or nodularity over these nerve points. All of these points, with one exception, are directly below the iliac crest.
Use these tender points as your indicators, allowing for a simple reassessment after treatment to see if you have quieted the involved nerves. I always mark the tender points so the patient and I both really know I am on the right spot.
Lyftogh4 (the originator of neuro-prolotherapy, now called perineural injection therapy) expanded this exam and looks for more irritated nerves, more laterally, also just below the iliac crest. Maigne's points on the superior cluneal nerve correspond with known fibro-osseous tunnels the nerves have to go through. The more lateral points probably do not have true fibro-osseous tunnels, but the nerve is at risk of impingement or irritation as it goes over the bony iliac crest.
How does one palpate these nerve points? Start with the patient either sitting in front of you or prone. I prefer to touch directly on the skin (the patient can just pull their shirt up and their pants a little ways down) just below the iliac crest.
I'll follow the iliac crest from medial to lateral, palpating just below the crest itself and feeling for palpable nodules that are tender. My impression is that these are not true trigger points; they are nerve-related tender points. I previously thought of them as muscle knots in the gluteal region. The superficial peripheral sensory nerves that begin in the TL and upper lumbar area pass through the iliac crest region and are impinged here. You may find more than one tender point along the crest.
From medial to lateral, we are first assessing the superior cluneal nerves, looking for a tender point about 7-8 cm lateral to the midline. These more medial nerves tend to come from L1-L3. A little more laterally, about 10-12 cm lateral to the midline, are the peripheral nerves originating from the lower thoracic segments. It is useful to remember that the courses of these nerves are variable.
Even farther laterally, over the superior aspect of the gluteus medius, you'll find the posterior cutaneous branch of the ilio-hypogastric nerve. Finally, as you round the corner anterior and medial to the ASIS, you will find the lateral femoral cutaneous nerve point. These two, the more lateral nerves, originate from the anterior sensory branches off of primarily L1 and L2. (Part 2 of this article will talk about addressing the anterior aspect of these nerves.)
The most obvious palpable points are just below the iliac crest. This probably has to do with the "crush" or impingement that occurs as the nerve crosses the bony iliac crest. I am talking as if these nerves are palpable. When they are inflamed and irritated, they are distinct and palpable. In a normal person's body, with no pain, they are much less evident.
To quote from Maigne's 1980 paper:5 "Low back pain arising from the apophyseal joints of the thoracolumbar region is common and is often erroneously attributed to pathologic changes in the low back. The diagnosis is made on pure clinical grounds. Classic signs are: a positive "iliac-crest point" test, a positive skin-rolling test, localized tenderness over a certain spinous process at the thoracolumbar junction and tenderness over the involved apophyseal joint."
Let's simplify this: First, find the thoracolumbar tender areas, indicating spinal dysfunction. Second, find the irritated nerve points below the iliac crest. Third, connect the dots. If a specific nerve is irritated, it will have tender and swollen areas all along its course. These areas or points tend to be a bit more subtle, a bit more difficult to identify. Your palpation follows a line from the involved vertebrae through the iliac crest point, and then down into the buttock and posterior and lateral hip. Skin rolling is another tool for assessing these changes in tissue texture.
Treatment Protocol
We'll keep it simple here. One, adjust the spine. Two, downregulate the nerve area itself via manual treatment and/or modalities. You are going to recheck both the spine and the points below the iliac crest after treatment. Part two of this article will go into more depth on treatment, and will include some exercise rehab concepts.
The spinal adjustment is so effective at immediately quieting the peripheral nerve. The downside of this immediate response: Adjusting can eliminate the tender peripheral indicators along the iliac crest. I often prefer to treat the nerve itself first, at least on the first visit, to evaluate what kind of direct treatment over the nerve is going to be most effective.
Over the peripheral nerve points, you can use modalities such as laser or LED light. The nerve is very superficial, so light reaches these easily. If you have a favorite electrical modality, see if it will quiet the nerve. Soft-tissue work is also useful.
Lyftogh claims deep-tissue work is contraindicated. I am not so sure. Whatever kind of soft-tissue work you prefer, trial it along these nerves. You are releasing the fascia that lines and surrounds the nerve. I often find my most subtle forms of soft tissue, such as counterstrain and gentle, indirect myofascial release, are most effective here.
As chiropractors, these peripheral tender points are not the only areas we will treat; they are primarily indicators of an upstream problem at the spine or exit points in the abdomen. Despite the secondary nature of these tender nerve points, they still need treatment. Any tissue that gets irritated becomes its own pain generator.
In my next article, I'll explore the more lateral nerves that come from the anterior rami, the ilio-hypogastric and lateral femoral cutaneous nerves; and discuss anterior palpation and anterior release strategies. I'll also talk about rehab: What muscles / movements are inhibited in this pain pattern? How can the patient normalize this through rehab exercises?
References
- http://sosas.us/professional-resources/.
- Triano JJ, Budgell B, Bagnulo A, et al. Review of methods used by chiropractors to determine the site for applying manipulation. Chiro & Manual Ther, 2013;21:36.
- "The Concept of Painful Minor Intervertebral Dysfunction" (summarizing Robert Maigne's work). French Society of Manual Medicine (Orthopedic and Osteopathic).
- From videos of Lyftogh's class, 2011; also Lyftogh J. Prolotherapy for recalcitrant lumbago. Australasian Musculskel Med, May 2008.
- Maigne R. Low back pain of thoracolumbar origin. Arch Phys Med Rehab, 1980 Sep;61(9):389-95.
Click here for more information about Marc Heller, DC.





