As a radiology consultant, I often am presented with plain-film radiographs by chiropractors concerned about the presence of a compression deformity. When there is a clear anterior wedge deformity, the question of "is this new or old?" is asked.
Compression fractures are the most common spinal fractures (47 percent).1 In addition, they are the most common types of fractures to occur in the lumbar spine.1-4 They most commonly occur at the T12-L2 segments.1-4 The typical mechanism is flexion and axial compressive force.1-4 The patient should have a history of significant trauma with the general mechanism described above, but only rarely will he or she present with neurologic deficit.1 The pain distribution typically originates from the involved segment posteriorly, and wraps around laterally and then forward toward the abdomen. Often the patient will prefer to stand - reducing the axial load on the spine - instead of sitting.1
If the patient is older than age 40, it is important to rule out pathologic weakening of the bone as an underlying etiology to the compression deformity.3,4 Potential pathologies to be considered include metastasis, myeloma, lymphoma, infection and, in the older age bracket, osteoporosis.1,2,3 Osteoporosis plays an important role in the prevalence of compression fractures.1 Compression fractures in the osteoporotic patient often will occur with only trivial injury.2 A thorough history with regard to the mechanism is imperative; the working diagnosis should include osteoporotic or pathologic compression. If there is a history of malignancy or infection, or if the films demonstrate osteoporosis or evidence of other underlying pathology, full laboratory investigation, as well as magnetic resonance imaging of the area of interest, should be performed. This will aid in ruling in or out the more aggressive causes of osteoporosis. MRI can distinguish between normal bone marrow, osteoporosis and other, more serious underlying disease infiltrating the vertebral body.2-4 Radiographic evidence of underlying pathology would include compression of both the anterior and posterior parts of the body, loss of one or both pedicles on the frontal view, loss of the sclerotic margin to the endplates, a moth-eaten pattern of bone destruction, and severe osteoporosis.2-4
Old vs. New Compression Fracture
Radiographically, it can be challenging to distinguish between old and new compression deformities; however, there are several plain-film findings that can assist the interpreter in making the distinction. An emphasis must be placed on the following radiographic findings with a history of trauma to make the diagnosis of a recent compression fracture.
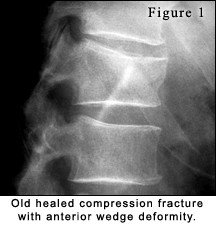 Vertebral body height: In the normal spine from T11 to L2, the vertebral segments are typically wedge-shaped anatomically. This normal appearance will present with approximately 10 percent to 15 percent or 1-3 mm less anterior body height compared to posterior body height.3 A common pitfall related to this is when normal morphology is confused with compression deformity. Loss of height at the anterior aspect of the vertebral body is the most common radiographic finding for compression fractures.2-4 Typically, disc material will remain intact and there will be no apparent loss of intervertebral disc height.2 In older, healed compression deformities, there is typically anterior wedge deformity greater than 15 percent. Some authors have stated that the degree of loss of height must exceed 30 percent to be detected on plain film.3 (See figure 1.)
Vertebral body height: In the normal spine from T11 to L2, the vertebral segments are typically wedge-shaped anatomically. This normal appearance will present with approximately 10 percent to 15 percent or 1-3 mm less anterior body height compared to posterior body height.3 A common pitfall related to this is when normal morphology is confused with compression deformity. Loss of height at the anterior aspect of the vertebral body is the most common radiographic finding for compression fractures.2-4 Typically, disc material will remain intact and there will be no apparent loss of intervertebral disc height.2 In older, healed compression deformities, there is typically anterior wedge deformity greater than 15 percent. Some authors have stated that the degree of loss of height must exceed 30 percent to be detected on plain film.3 (See figure 1.)
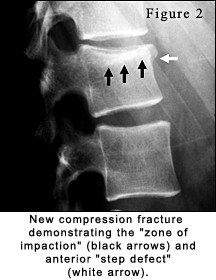 Step defect and zone of impaction: In the acute injury phase (within two months), there is the presence of the "step defect" and the "zone of impaction."3,4 (See figure 2.) The "step defect" is seen on the lateral projection and represents failure of the anterior superior cortex of the vertebral body. As the superior endplate gets compressed and shifts forward, the anterior cortex fails and creates a step.3,4 It represents the anterior displaced corner of the endplate. In subtle compression deformities, this may be the only radiographic finding.3 The "zone of impaction," also referred to as the zone or line of condensation, will present radiographically as a dense white band just below the compressed endplate. This finding is not always present and represents a region of impacted bone.3,4 If either of these two finding is present, it confirms the presence of an acute traumatic compression fracture less than two months old. After that time period, with healing, these findings will no longer be visible.3
Step defect and zone of impaction: In the acute injury phase (within two months), there is the presence of the "step defect" and the "zone of impaction."3,4 (See figure 2.) The "step defect" is seen on the lateral projection and represents failure of the anterior superior cortex of the vertebral body. As the superior endplate gets compressed and shifts forward, the anterior cortex fails and creates a step.3,4 It represents the anterior displaced corner of the endplate. In subtle compression deformities, this may be the only radiographic finding.3 The "zone of impaction," also referred to as the zone or line of condensation, will present radiographically as a dense white band just below the compressed endplate. This finding is not always present and represents a region of impacted bone.3,4 If either of these two finding is present, it confirms the presence of an acute traumatic compression fracture less than two months old. After that time period, with healing, these findings will no longer be visible.3
Soft-tissue findings: In addition to bony findings, there can be the presence of soft-tissue edema in the paraspinal region. Also possible is abdominal ileus, in which bowel motility is reduced and it begins to fill with air. Both findings indicate severe trauma and the possibility of associated fracture.3
Management
Simple compression fractures are considered stable; those that are uncomplicated can be managed appropriately in the chiropractic setting. The first principle of management is immobilization of the fracture to allow proper healing.1 For compression fractures, this process takes a minimum of four weeks in the young adult, and approximately six to eight weeks in older adults.1 It is important that applied forces or movements be minimized in the first three to four weeks of fracture healing (and longer in older patients).1 There is an expectation that posttraumatic deformity will be present.1,4 Such an area of deformity will be a future site for degenerative joint disease as well as altered spinal motion, due to changes in joint biomechanics.1-3
Occasionally, in severe injury there may be the presence of disc herniation and neurologic symptoms.1 In addition, there can be more severe compressions that can complicate management. In the event of greater than 40 percent loss of anterior vertebral body height, there may be the need for surgical intervention and posterior stabilization.2 When complications such as these arise, additional imaging such as computed tomography and magnetic resonance imaging often are acquired.1-3 Due to medical-legal concerns and the comfort level of the treating chiropractor, it is not unwise for an orthopedic referral to be made, particularly in complicated cases.1 Once past any complicating issues and after the initial fracture healing time frame of four to six weeks, chiropractic management may be appropriate. There is a tremendous amount of potential benefit to the patient from spinal manipulation and soft-tissue rehabilitation applied to well-healed compression fractures.
Conclusion
When a patient presents with a history of trauma and an anterior wedge deformity of the vertebral body, there are radiographic findings that assist in determining whether the doctor is dealing with recent or old compression fractures. Once the clinician has ruled out underlying pathology, including osteoporosis and more serious complications of traumatic compression fracture, these patients can be managed effectively in the chiropractic setting.
References
- Bassano J, Schultz G. Spinal fractures: a clinico-radiographic approach. Topics in Clin Chiro 1998;5(3):16-26.
- Resnick, D, Niwayama, G. Diagnosis of Bone and Joint Disorders, 3rd edition. Philadelphia: W.B. Saunders, 1995.
- Yochum T, Rowe L. Essentials of Skeletal Radiology, 3rd edition. Baltimore: Williams & Wilkins, 2005.
- Marchiori D. Clinical Imaging With Skeletal, Chest and Abdomen. St. Louis: Mosby, 1999.




