Core stability refers to the activation of the muscles that stabilize the lower back, including the multifidi, transverse abdominals and pelvic floor. These core muscles are key stabilizers of both the lumbar spine and the pelvis.
Evaluating Core Stability
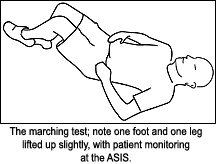
When you evaluate your low back patients, it is critical to assess core stability. I'll outline two basic ways to do this. The "marching" test is a variation on the active straight-leg-raise test.1,2 It is done supine and has the advantage that the patient can self-assess in follow-up. Have the patient supine with the legs standing (feet flat on floor, knees bent). Have the patient place their index fingers over the ASIS bilaterally. Stand at the side of the table and place your own thumbs over the patient's index fingers, so you can monitor. Have the patient slowly lift the left leg by lifting the left foot up 2 or 3 inches. Does the left ASIS jump, moving suddenly superior and posterior? Observe the abdomen. Does the abdomen bulge when the patient lifts the leg? Does the pelvis shift with one side dropping toward the table, and the other side coming anterior?
Change your position, putting a hand under the spine. Does the patient extend their spine and fire their erectors while lifting the leg? All of these are indicators of instability. Repeat the test on the right side and compare. If the patient knows how to "fire their core," how to abdominally co-contract, have them repeat these motions with their core activated. Are the results different?
 What are you looking for here? The ASIS is not a bone sticking out in space. It is the anterior portion of the ilium, and motion here indicates motion at the sacroiliac (SI) joint. An ideal result is a minimal, slight, gradual movement of the ASIS superior and posterior, with no abdominal bulging, and no shift, and no hyperactivation in the back. If the ASIS jumps superior/posterior, or if any one of these aberrant motions occurs at the beginning of the marching movement, the pelvis on that side has excessive unguarded movement. This correlates with an unstable SI joint and affects the entire lumbopelvic girdle. Imagine what is happening with the patient when they move suddenly, walk, or rise from a seated position. The muscles and/or ligaments are not properly supporting the SI joint. Sometimes, the abnormal movement occurs on only one side; sometimes, both sides have excessive motion. As in any motor skill, after you have done this test several times, your assessment skills will improve.
What are you looking for here? The ASIS is not a bone sticking out in space. It is the anterior portion of the ilium, and motion here indicates motion at the sacroiliac (SI) joint. An ideal result is a minimal, slight, gradual movement of the ASIS superior and posterior, with no abdominal bulging, and no shift, and no hyperactivation in the back. If the ASIS jumps superior/posterior, or if any one of these aberrant motions occurs at the beginning of the marching movement, the pelvis on that side has excessive unguarded movement. This correlates with an unstable SI joint and affects the entire lumbopelvic girdle. Imagine what is happening with the patient when they move suddenly, walk, or rise from a seated position. The muscles and/or ligaments are not properly supporting the SI joint. Sometimes, the abnormal movement occurs on only one side; sometimes, both sides have excessive motion. As in any motor skill, after you have done this test several times, your assessment skills will improve.
The beauty of this test is that the patient can self-monitor. The patient can learn how to fire their core properly in a way that stabilizes the pelvis. The patient then can practice this, as an exercise, doing the same foot lift as described above, and assess their stability. More advanced exercises would involve lifting the leg further or performing a bicycle-type motion with the leg. The basic idea is to challenge the pelvis by moving the leg, keeping pelvic movement minimal and under control through a sustained, tonic, gentle contraction of the core.
One more test, especially for those trained in motion palpation. The initial evaluation for the SI that I learned from Leonard Faye 28 years ago was the Gillet test, or a standing marching test. I was taught to look for a lack of motion. This same test has been re-evaluated by a physical therapist as part of her doctoral research.3,4,5 She calls this test a load transfer, and instead of looking for hypomobility, she is looking for functional hypermobility, or instability.
How is this done? The patient is standing in front of you. You can assess left-side instability by touching the bottom of the left PSIS and the left side of the sacrum at the same horizontal level. Have the patient slightly lift the right foot off the ground. What happens to the left SI when you load it, make it bear all of the weight, by lifting the right foot slightly? In a normal subject, the left PSIS, the left inominate, should posteriorly rotate along with the sacrum. In motor pathology, when the muscles are not stabilizing properly, you'll see and feel the left PSIS rotate anterior in relation to the sacrum. These rotations are in the plane of the SI joint. Test both sides. On the side of dysfunction, the patient also will have an inability to stand with ease on that leg and will sway. This test is another excellent way to test both function of the core stabilizing muscles and SI functional stability. The retest: Once the patient knows how to properly fire their core, they will be able to stand on one leg more easily and the PSIS will move normally.
Core Stability Exercises
Here is my view of the basics on core stability exercises: Teach the patient to maintain a neutral lordosis while firing three sets of muscles - the pelvic floor from below, the transverse abdominals, and the multifidi. There are several common errors in firing the core: The patient goes into a posterior pelvic tilt, flexing their spine, or the patient overfires their larger lumbar extensors, which is obvious on palpation or by observing arching of the low back. You also may observe bulging of the abdomen.
Core stabilization should be a low-grade, mild contraction of tonic muscles which can be held for a long time (20 seconds to several minutes), not just a sudden contraction. Teach your patient to do this in multiple positions; teach them to incorporate this firing of the core into any other exercises and teach them to fire their core during activities of daily living.
I want to add one more advanced or specific aspect of core stabilization here. I use this with the supine marching test.6 First I teach the basics of firing the core, and then I have the patient hold a mild contraction while lifting the leg. If the patient still has excessive ASIS motion or other motor errors while firing their core, have them add one more component. I'll describe several ways of determining what exact component to add. First, slide your hand under the patient's back as they fire their pelvic floor while supine. There should be a slight contraction of the multifidi bilaterally. If the right side feels more atrophied, try this: Have the patient attempt to fire the weaker side - in this case, the right - in the back, and pull in or fire the opposite left transverse abs. In other words, you are asking the patient to fire across a diagonal. Another way to say this is to ask the patient to "Pull your right PSIS (or right posterior pelvis) toward your left, lower abdomen."
The patient may overfire and twist the whole pelvis. If so, tell them it's more subtle, just a slight firing of the muscles with no gross movement. Retest, having the patient monitor their ASIS as they lift the leg. If this improves the pattern, the patient needs to modify their core firing by focusing on this diagonal. If this doesn't help, try the opposite diagonal. You also could have them try the right posterior and right anterior together, or the left posterior and left anterior together. Generally it's one or the other diagonal, sometimes with an emphasis more on the front or back. This may sound a bit complex at first, but once you get it and once your patient gets it, it's fairly straightforward.
Here's another protocol for asessing which muscles need further support, from Diane Lee, PT.7 This involves focusing on the same muscles, but having the doctor passively create the stability through compression. This passive compression can be done unilaterally or bilaterally, across the lower abdomen, or across the SI area.
In the front, you take a broad contact from the ASIS medially, pressing medially to reinforce the transverse abs, and then retest. In the back, your broad contact would press medially from the gluteus medius across to the PSIS, reinforcing the lower multifidi. Diane Lee has a special SI belt, called the compressor, which includes extra elastic reinforcement pieces that can be velcroed to the belt to help retrain or reinforce the needed motions. You also could use an ordinary SI belt and add some elastic tape, going lateral to medial to reinforce the directions you want to enhance.
Training the core is worth learning and doing. This may be the most significant activity you can teach your chronic lower back patients. I don't believe, and the literature does not support, the idea that adjustments, whether high velocity or low force, can correct muscular instability fully. When there is a muscular contribution to the problem it needs a muscular solution. Ideally, when the patient raises their leg, whether in these tests or in real life, the core muscles automatically fire, just enough to stabilize the low back and pelvis. It's not always easy or simple for the patient, especially your "motor morons," to get this. Teaching basic rehab can help you stabilize and get results with your most difficult patients.
References
- Liebenson, Craig. Sacroiliac dysfunction and lumbopelvic instability. Dynamic Chiropractic, Aug. 24, 1998. www.chiroweb.com/archives/16/18/03.html.
- Liebenson, Craig. Vleeming's active SLR test as a screen for lumbo-pelvic dysfunction. Dynamic Chiropractic, Feb. 24, 2003. www.chiroweb.com/archives/21/05/13.html.
- Hungerford, B, et al. Evidence of altered lumbo-pelvic muscle recruitment in the presence of sacroiliac joint pain. Spine 2003;28:1593-1600.
- Hungerford, B, et al. Altered patterns of pelvic bone motion determined in subjects with posterior pelvic pain using skin markers. Clinical Biomechanics 2004;19:456-464.
- Hungerford, B. Synopsis of Analysis of Functional Load Transfer Through the Pelvis: Patterns of Intra-pelvic Motion and Muscle Recruitment for Pelvic Stability, Dr. Hungerford's PhD thesis.
- Lowengart, Ruth, Ramona Horton. The Southern Oregon Orthopedic Study Group, 2005, and personal communications.
- www.dianelee.ca.
Click here for more information about Marc Heller, DC.





