Introduction
In our society, chiropractic physicians provide valuable services in a primary care setting. Patients often seek chiropractic care without a medical referral or having undergone prior medical evaluation.
The utilization of advanced diagnostic protocols provides valuable insight into the care of patients. Magnetic resonance imaging (MRI) provides diagnostic utility that is extremely important in clinical practice. The pathophysiologic affects of the chiropractic subluxation and its sequelae are readily visualized via MRI.
MRI is extremely important in defining pathologic states that may represent possible contraindications to chiropractic care. It provides a glimpse into the physiologic mechanisms that reflect spinal integrity.
The following is a case that illustrates the utility of MRI in chiropractic practice. While the patient presented with complaints that are readily seen in the chiropractic setting, MRI allowed visualization of a significant and potentially life-threatening clinical entity.
Case Report
 A 37-year-old female presented to our office in acute pain and difficulty ambulating. She reported an insidious onset over two to three days of increasing hip, buttock and leg pain with radiation to the foot. No recent trauma was reported. She had difficulty bearing weight on the affected extremity. These symptoms progressively worsened without relief. The patient reported no urinary or bowel incontinence. She denied any abdominal pain.
A 37-year-old female presented to our office in acute pain and difficulty ambulating. She reported an insidious onset over two to three days of increasing hip, buttock and leg pain with radiation to the foot. No recent trauma was reported. She had difficulty bearing weight on the affected extremity. These symptoms progressively worsened without relief. The patient reported no urinary or bowel incontinence. She denied any abdominal pain.
The patient's past medical history was significant for heart disease. Due to a heart valve abnormality, she received a mechanical Starr-Edwards type heart valve surgical replacement. Her medications included Coumadin therapy monitored by her cardiologist. Her Coumadin levels and clotting prothrombin times were reported to be within normal limits.
On inspection, the patient was nearly unable to bear weight on the affected extremity. Her vital signs were within normal limits. She was afebrile. Abdominal evaluation was normal. Peripheral vascular evaluation was without abnormality.
Physical examination revealed restricted and exquisitely painful hip range of motion. Palpation revealed acute tenderness of the deep gluteal and piriformis musculature. Nerve root tension signs, including SLR and seated SLR, provoked hip and leg pain. The patient exhibited positive Fabere, Laguere and Hibbs tests. Kemp's test was negative. Valsalva was negative. Neurologic evaluation revealed 0/5 Achilles deep tendon reflex and +3/5 weakness of the foot plantar flexion on the affected side. Pathologic reflexes were absent.
Chiropractic subluxation was noted, affecting the sacroiliac on the affected side. Lumbar spine, AP pelvis and hip X-rays revealed no osseous or soft-tissue pathology, and no evidence of trauma, fracture or dislocation.
 Differential diagnosis included: synovitis of the hip; fracture; avascular necrosis of the femoral head; piriformis syndrome; and lumbar radiculitis. Chiropractic subluxation of the sacroiliac joint was identified. The patient's progressively increasing pain and inability to bear weight on the affected extremity mandated advanced diagnostic imaging. The patient was referred for MRI evaluation of the hips without contrast.
Differential diagnosis included: synovitis of the hip; fracture; avascular necrosis of the femoral head; piriformis syndrome; and lumbar radiculitis. Chiropractic subluxation of the sacroiliac joint was identified. The patient's progressively increasing pain and inability to bear weight on the affected extremity mandated advanced diagnostic imaging. The patient was referred for MRI evaluation of the hips without contrast.
Prior to performing the MRI, the presence of the Starr-Edwards mechanical heart valve mandated consultation with the attending radiologist to determine the safety and appropriateness of MRI for this patient. He confirmed that the patient's prosthesis was absent of ferromagnetic properties and that it was safe to perform an MRI of the hips. The radiologist made the final decision to proceed with the MRI.
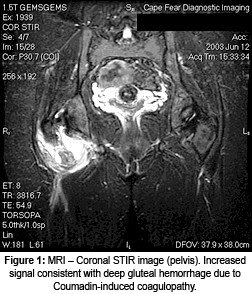
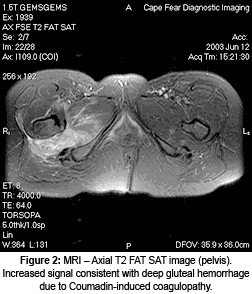
The MRI examination provided a definitive diagnosis. A large, acute hematoma was visualized deep within the buttocks, affecting the gluteus maximus, medius, piriformis and adductor magnus muscles (see figures 1 and 2). The proximity of the hematoma to the sciatic nerve was visualized. No bony or joint abnormalities were noted. The patient was transported to our local hospital emergency department for treatment of the visualized internal hemorrhage.
Laboratory tests confirmed that the patient suffered an internal hemorrhage due to a coagulopathy related to poorly managed Coumadin levels. She was provided supportive care during her three-day hospital stay and recovered fully.
Discussion
This case contains numerous factors that are interesting and instructive. While the patient exhibited history, signs and symptoms commonly seen in the chiropractic office, other more emergent problems were present. Due to poor Coumadin management, the patient suffered preventable morbidity.
The demonstrated hemorrhage produced orthopedic symptoms that confounded a true diagnosis. The patient's medical history of poorly managed Coumadin levels was important. The differential diagnosis required careful assessment and decision-making.
The use of advanced diagnostic imaging was critical in this case. It was necessary to ensure that the patient's prosthesis did not pose a contraindication to MRI. Rapid identification and coordination of integrated services provided the patient an optimal result.
Conclusion
This case illustrates the importance of careful history and examination. Patients' conditions progress, change, improve and deteriorate based upon their health care status. It is requisite that caregivers take a logical approach to clinical decision-making for the people in their charge. The use of MRI was extre-mely important in this case.




