I present to you a new patient; a 57-year-old male, whose chief complaint is constant pain in the lower back. The pain started this morning, and is not improving. The patient has been to the ER and worked up for possible infection, but was sent home with a diagnosis of strain/sprain.
History is as follows: The day before, the patient was retrieving a palm frond that had fallen on the roof of his house. He accidentally cut his hand on the rain gutter as he was pulling the frond off the roof. He just put some duct tape on the cut to stop the bleeding. The next morning, the patient woke up with excruciating back pain. His wife took him to the ER because he was in so much pain. Lab studies were done at the ER; they were normal (CBC and UA). X-rays of the lumbar spine were normal for patient's age and the wound was unremarkable. Patient was told he must have a strain/sprain because his labs were normal and the X-ray study was normal. Patient still is in marked discomfort, so his wife decides to take him to a chiropractor. The patient's symptoms are constant lower back pain that radiates into the groin. His symptoms are so acute that you cannot perform any orthopedic tests.
What are you going to do for this patient? I am discussing this case with you because the chiropractor who saw this patient literally saved the man's life. Even though the patient had just come from the ER with normal labs, the DC sent the patient right back to the ER, making certain the lab studies were repeated. The second time the labs were done, the patient's ESR was high, his WBC count was higher and he was beginning to develop a fever. An MRI was done; it demonstrated changes at the L4-5 level, indicative of a discitis. By the time the patient was admitted to the hospital, he was septic. Apparently, the patient infected himself by sucking on the cut of his hand to stop the bleeding and did not clean the wound sufficiently before bandaging it with duct tape.
The term discitis simply indicates there is an inflammatory reaction involving the intervertebral disc. It almost always is due to an infection, either bacterial or fungal. The infection frequently involves the adjacent vertebral bodies, resulting in osteomyelitis, since the disc and vertebrae share the same pathophysiology. Another term used to describe this entity is spondylodiscitis. The infection often can cause debilitating neurologic injury and morbidity if diagnosis and treatment are delayed. The lumbar region most commonly is affected, followed by the cervical spine and then the thoracic spine.
The infection ordinarily does not originate in the vertebra or disc unless there is a history of recent surgery or an invasive procedure. The infective agent usually enters through a wound and spreads via the bloodstream. In the U.S., the incidence of discitis is estimated to be approximately one to two in 100,000, depending on the study. This rate is similar internationally, with the exception of some areas of Africa, where it has been reported as high as 11 percent of all patients with back pain. Mortality has been reported as between 2 and 12 percent, which is a significant range that I cannot explain. There is a higher incidence in males to females (2:1 ratio), with a peak incidence at the mean age of seven years, which then decreases until middle age. There is a second peak in incidence at approximately 50 years of age.
Pyogenic spondylitis involves one or more of the epidural components of the spine. The vertebral bodies most often are affected, but the intervertebral discs, epidural space and paraspinous soft tissues might be involved. A broad spectrum of infectious agents can cause pyogenic spondylitis, including fungus, bacteria or parasites. However, Staphylococcus aureus is the most common etiology in adults. Routes of infection include hematogenous spread, contiguous spread, in direct inoculation. The most common cause is systemic bacteremia, usually from a cutaneous, urinary or pulmonary infection. Less common is direct contamination from diagnostic procedures, open wounds, penetrating foreign bodies or surgery.
 In adults, the infection typically begins in the subchondral portion of the vertebral body and subsequently spreads to the disc. Children have richly vascularized intervertebral discs, and the infection may begin here before spreading to the vertebral bodies. The laboratory tests can be unreliable, especially early on in the infective process. The ESR and C-reactive protein are the most consistent laboratory abnormalities. Plain films usually are normal for the first eight to 10 days. The plain-film findings, which include loss in disc height and endplate erosions, often are very subtle and are not detected until later. CT also might be normal early on and demonstrate narrowed disc space, cortical bone loss and paraspinous soft-tissue mass.
In adults, the infection typically begins in the subchondral portion of the vertebral body and subsequently spreads to the disc. Children have richly vascularized intervertebral discs, and the infection may begin here before spreading to the vertebral bodies. The laboratory tests can be unreliable, especially early on in the infective process. The ESR and C-reactive protein are the most consistent laboratory abnormalities. Plain films usually are normal for the first eight to 10 days. The plain-film findings, which include loss in disc height and endplate erosions, often are very subtle and are not detected until later. CT also might be normal early on and demonstrate narrowed disc space, cortical bone loss and paraspinous soft-tissue mass.
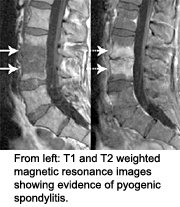
MRI is the most reliable modality for demonstrating pyogenic spondylitis. The characteristic findings are: In the T1 weighted images, there is a loss of disc height, a decreased signal in the vertebral bodies due to edema within the marrow, a paraspinous abscess, and epidural extension. Associated meningeal inflammation may be demonstrated. The T2 weighted images demonstrate an increased signal in the affected disc space and vertebral bodies.
Antibiotic treatment must be tailored to the isolated organism and any other sites of infection. Complications include neurologic deficits in 13 percent to 40 percent of patients, especially those with diabetes or other systemic illnesses. Long-term antibiotic therapy may lead to ototoxicity or renal toxicity. Most patients are cured by a treatment protocol of antibiotics, either alone or in combination with surgery. Fifteen percent of patients experience permanent neurologic deficits. Recurrences of infection take place in 2 percent to 8 percent of patients.
Getting back to our patient, he was treated appropriately and presently, three months from initial onset he still is experiencing lower back pain and is unable to stand or sit for long periods of time. Walking also is difficult, but prognosis is good that he will recover completely. I think that if his wife did not take him to the chiropractor, he could have suffered, at the very least, irreversible neurological damage. My hat goes off to the DC for his sound evaluation and referral.
Resources
- Maiuri F, Iaconetta G, Gallicchio B. Spondylodiscitis: clinical and magnetic resonance diagnosis. Spine, August 1997;22(15):1741-6.
- Khan IA, Vaccaro AR, Zlotolow DA. Management of vertebral diskitis and osteomyelitis. Orthopedics, August 1999;22(8):758-65.
Click here for more information about Deborah Pate, DC, DACBR.





