An abdominal aortic aneurysm (AAA) occurs when the aorta balloons outward or expands in size. AAAs usually occur in men over 60, but it can happen to virtually anyone at any age regardless of gender.
Symptoms and Diagnosis
AAAs can be difficult to diagnose because they develop very slowly and may be completely asymptomatic. AAA is a medical emergency and less than 80 percent of patients survive once the aorta has ruptured. Sudden death can occur when the aneurysm ruptures or result in the following symptoms:
- Shock
- Dizziness
- Rapid heart rate
- Clammy skin
- Nausea
- Vomiting
- Pain in the abdomen and back that may spread to the groin, buttocks and legs
- Pain can be sudden, severe, persistent or constant
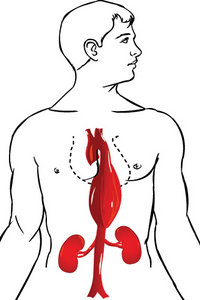 Abdominal examination may reveal a stiff or rigid abdomen, a lump or mass in the abdomen, and a pulsating sensation upon palpation. A vascular exam of the pulses in the legs is also warranted. Diagnostic imaging, which may include a lateral lumbar X-ray, abdominal ultrasound, angiogram or abdominal CT scan, many times identifies the AAA.
Abdominal examination may reveal a stiff or rigid abdomen, a lump or mass in the abdomen, and a pulsating sensation upon palpation. A vascular exam of the pulses in the legs is also warranted. Diagnostic imaging, which may include a lateral lumbar X-ray, abdominal ultrasound, angiogram or abdominal CT scan, many times identifies the AAA.
If the AAA is small enough, it should be monitored every six months by ultrasound to see if it is enlarging. Once the AAA is larger than 2 inches, surgery is recommended to repair the aorta. Repair can be done by a traditional graft with man-made material or a procedure called endovascular stent grafting, which does not require making an incision in the abdomen. Outcomes are usually excellent when the surgery is performed correctly.
The Infection Connection
Recommendations for prevention usually include eating a "heart-healthy diet," not smoking, exercising and reducing stress. However, one of the most overlooked aspects of AAA is the infection connection and the hypothesis that AAA is an autoimmune disease. Microbes can trigger autoimmune disease by a mechanism known as molecular mimicry, whereby microbial antigens share amino- acid sequence homologies with host tissue.
The bacteria Chlamydia pneumoniae has been implicated in various autoimmune diseases such as multiple sclerosis and Alzheimer's, as well as atherosclerosis, vasculitis and now AAA. Lindholt, et al., found that 16 of 17 AAA wall samples showed cross-reactivity with Chlamydia pneumoniae outer membrane proteins and human immunoglobulin. The authors conclude, "This might indicate that AAA is an autoimmune disease, perhaps triggered by an initial Chlamydia pneumoniae infection."
Pupka, et al., evaluated 60 patients who underwent surgery due to AAA; the group included 30 patients with asymptomatic aneurysm and 30 with ruptured aneurysm. The control group was comprised of 30 organ donors. Surgical specimens derived from aneurysm or aorta fragments were investigated for Chlamydia pneumoniae DNA using PCR.
In asymptomatic aneurysms, DNA was found in nine cases (29 percent), and in ruptured aneurysms in 14 cases (49 percent). In the control group, C. pneumoniae DNA was not detected in an aortic wall. A large number of aneurysm infections implies C. pneumoniae's role in proteolysis and degradation of the aneurysm wall. The biological effect of this process may cause an enlargement of the aneurysm.
Xiong, et al., evaluated the presence of Chlamydia pneumoniae in all three layers of the abdominal aorta including the intima, media and adventitia in 20 patients with AAA. The positive rate for C. pneumoniae was 100 percent (all 20 patients).
Borrelia burgdorferi is the bacteria that causes Lyme disease and has also been implicated in AAA. Hinterseher, et al., found that 34 percent of the 96 patients they studied with AAA tested positive for Borrelia burgdorferi. They did not find B. burgdorferi in the aortic wall, however, via PCR and thus hypothesized autoimmunity via molecular mimicry, as Lindholt, et al., suggested previously about Chlamydia pneuomoniae.
Chlamydia pneumoniae and Borrelia burgdorferi are both gram-negative bacteria that have the ability to enter vascular tissue and create chronic, low-grade inflammation. Their role in inducing autoimmunity via molecular mimicry has been established. Testing for Chlamydia pneumoniae can be done in serum via IgG, IgM and IgA antibodies, as well as polymerase chain reaction (PCR) for identification of microbial DNA. Borrelia burgdorferi is initially tested via ELISA and then confirmed with a Western blot. Borrelia testing is also available through culture and PCR.
Prevention and treatment by diagnosing and addressing chronic infectious involvement in AAA may yield improved quality of life and inhibition of AAA progression when found to be stable or slow-growing. A good history, examination and diagnostic testing just may save a life.
References
- Lindholt JS, Støvring J, Østergaard L, Urbonavicius S, Henneberg EW, Honoré B, Vorum H. Serum antibodies against Chlamydia pneumoniae outer membrane protein cross-react with the heavy chain of immunoglobulin in the wall of abdominal aortic aneurysms. Circulation, 2004 May 4;109(17):2097-102.
- Pupka A, Skóra J, Kaluza G, Szyber. The detection of Chlamydia pneumoniae in aneurysm of abdominal aorta and in normal aortic wall of organ donors. P. Folia Microbiol (Praha), 2004;49(1):79-82.
- Xiong F, Zhao JC. Quantification and location of Chlamydia pneumoniae-specific antigen in the walls of abdominal aortic aneurysms. Ann Vasc Surg, 2011 Feb;25(2):256-63.
- Hinterseher I, Gäbel G, Corvinus F, Lück C, Saeger HD, Bergert H, Tromp G, Kuivaniemi H. Presence of Borrelia burgdorferi sensu lato antibodies in the serum of patients with abdominal aortic aneurysms. Eur J Clin Microbiol Infect Dis, 2012 May;31(5):781-9.
Dr. Nikolas Hedberg, a 2003 graduate of Texas Chiropractic College, is a board-certified chiropractic internist and the founder of the Immune Restoration Center in Asheville, N.C., where he focuses on treating infectious and autoimmune disease. Contact him via his website, www.infectionconnection.net.




