We have all had acute patients enter our offices listing laterally to the side at the level of the lumbar spine or expressing pain on lateral lumbar bending. There are many possibilities as to why they are in this position, including a compensatory reaction to a herniated disc or to a spasm due to a malfunction in the myofascial system.
Anatomical Perspective
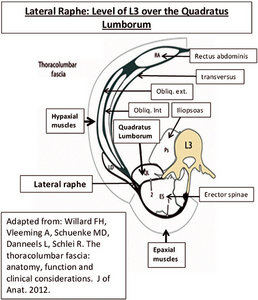
Lateral to the erector spinae muscles, the anterior and posterior layers of the thoracolumbar fascia (TLF) fuse to form the lateral raphé, which extends inferiorly from the iliac crest to the 12th rib superiorly.1 In the lower back, the anterior or hypaxial muscles consist of the rectus abdominis, transversus abdominis, quadratus lumborum (QL) and psoas muscles. (Figure 1)
The epaxial muscles consist of the erector spinae and the transversospinal muscles (including the multifidus, semispinalis and rotators). The hypaxial muscles are separated from the epaxial muscles by a septum, which in humans corresponds to a layer attaching from the transverse processes and covering the erector spinae forming the anterior layer of the TLF.
 Some authorities refer to this anterior layer as the middle layer of a three-layered structure of the TLF. Both the two- and three-layer TLF proponents accept the posterior layer, but Carla Stecco2 believes in a two-layered model of the TLF. She finds that in the three-layer model, the anterior layer that covers the iliopsoas and quadratus lumborum has macroscopical and histological features completely different from the thoracolumbar fascia. The anterior fascia over the quadratus lumborum is thin and not able to transmit tension from the various muscles to the thoracolumbar spine, which is one of the main roles of the TLF.
Some authorities refer to this anterior layer as the middle layer of a three-layered structure of the TLF. Both the two- and three-layer TLF proponents accept the posterior layer, but Carla Stecco2 believes in a two-layered model of the TLF. She finds that in the three-layer model, the anterior layer that covers the iliopsoas and quadratus lumborum has macroscopical and histological features completely different from the thoracolumbar fascia. The anterior fascia over the quadratus lumborum is thin and not able to transmit tension from the various muscles to the thoracolumbar spine, which is one of the main roles of the TLF.
From a functional point of view, the anterior layered fascia in the three-layer model is more closely related to the fasciae of the pelvis (iliopsoas fascia) and of the abdomen (epimysial fascia of the transversus abdominis muscle), rather than the thoracolumbar fascia. Stecco finds that in the three-layered model, "the fascia on the anterior aspect of the QL is considered to be an extension of the fasciae from the abdominal wall, particularly of the transversus abdominis muscle. The transversus abdominis muscle together with its fascia connect the rectus with the quadratus lumborum and psoas muscles, joining the hypaxial muscles." So, for the purpose of this article, the anterior layer is the one that extends from the transverse processes between the quadratus lumborum and erector spinae.
The lateral raphé is a thickened complex of dense connective tissue and represents the junction of the hypaxial myofascial compartment with the paraspinal sheath of the epaxial muscles. Along this raphé, all the forces produced by the muscles inserted into the anterior and posterior layers of the TLF converge. The lateral raphé has the role of redistributing these muscular tensions into both layers of the TLF, diffusing the tension so it is not localized to only a few vertebrae.3
A Treatment Strategy
Using soft-tissue methods directed at reducing the density of tight fascia in the quadratus lumborum area (also affecting the lateral raphé) may diminish lumbar pain and restore both lateral and often other limited ranges of motion by normalizing fascial tension between the hypaxial and epaxial muscles.
Let's review a local treatment taught in fascial manipulation that might help an acute or chronic lower back complaint. However, it must be emphasized that this particular point ["lateral lumbar, (La-lu)"] is never used by itself with regards to fascial treatment. Treating a lateral fascial sequence is often combined with, in this type of problem, to fascial dysfunction anywhere along this lateral line, possibly found anywhere from the ankle (knee, hip etc.) to the cervical spine.
 La-lu may be compensatory to a past fascial disruption proximal or distal to it. It has been found that to complete treatment in a balanced state, in this case it would be imperative to treat La-lu on the opposite, antagonistic side. The antagonistic side of a problem is usually under stress, compensating for the agonist side.
La-lu may be compensatory to a past fascial disruption proximal or distal to it. It has been found that to complete treatment in a balanced state, in this case it would be imperative to treat La-lu on the opposite, antagonistic side. The antagonistic side of a problem is usually under stress, compensating for the agonist side.
As stated in previous articles in DC and elsewhere, fascia has been found to be a sensory organ, since muscle spindle cells that influence the tone, velocity of stretch and awareness of muscle position are actually in the fascia (especially the perimysium). Since spindle cell fibers must be stretched during muscle contraction for normal feedback to the central nervous system, it becomes important to ensure normal gliding of the fascia during active or passive muscle motion. Restricted gliding of the fascia would inhibit normal spindle cell stretch and therefore interfere with proprioception. A state of muscle incoordination would result.
In terms of treatment using this particular point, we are not, as discussed above, including the kinetic fascial chain, but there are some interesting things to know that might be helpful with some of your own techniques. It has been found that hyaluronic acid (HA) molecules, which provides the fluid medium between muscle fibers and joints, become entangled, creating a gel-like substance preventing normal muscle-fascial glide.4
McCombe, et al.,5 found HA concentrated on the inner surface of the deep fascia, which is in contact with the underlying muscle. The deep fascia is a multilayered structure of dense and loose connective tissue, which produces a gliding interface in conjunction with the epimysium of the muscle. It has also been found that pressure and increased temperature restores the molecular balance and returns HA to the fluid state. In performing fascial manipulation, we feel for a density of the fascia, which is usually sensitive to the patient.
A recent study6 evaluated three manual therapy motions (perpendicular vibration, tangential oscillation and constant sliding) to determine how each affects the flow characteristics of HA below the fascial layer. It was found that perpendicular vibration and tangential oscillation (forms of friction massage) were better than the use of a constant sliding motion in increasing the fluid pressure of HA.
The first two methods generated more fluid between the muscle and the fascia. The thickness between the two fascial layers increased and improved the gliding between the fascia and the muscles.
In the photo, the patient is on his side with his top knee and leg forward over the bottom knee to help open up the lateral side. The clinician uses the point of his elbow over the quadratus lumborum, pressing toward the erector spinae. Usually the area will be tender to the patient. With the elbow, you can palpate obliquely inferior and superior to feel the most densified area and use a friction massage technique. Graston Technique instruments could also be used. Always friction within the tolerance of the patient.
A study7 that evaluated the time required to modify apparent fascial density in 40 patients with low back pain, taking into consideration the symptoms and patient physical characteristics, found that the mean time to halve the pain was 3.24 minutes. In subjects with symptoms present for less than three months (subacute), the mean time was 2.58 minutes. In subjects with chronic pain over three months, the mean time was 3.29 minutes.
Usually after treatment the range of motion improves. Treating the lateral side with this method may also restore limited motion in other directions. I have seen a patient's normal posture restored after one visit.
References
- Bogduk N, Macintosh JE. The applied anatomy of the thoracolumbar fascia. Spine, 1984;9(2):164-70.
- Stecco C. An Atlas of the Human Fascial System. Elsevier (in print), 2014.
- Schuenke MD, Vleeming A, Van Hoof T, Willard FH. A description of the lumbar interfascial triangle and its relation with the lateral raphe: anatomical constituents of load transfer through the lateral margin of the thoracolumbar fascia. J Anat, 2012; 15.
- Stecco C, Stern R, Porzionato A, et al. Hyaluronan within fascia in the etiology of myofascial pain. Surg Radiol Anat, 2011;33:891-896.
- McCombe D, Brown T, Slavin J, Morrison WA. The histochemical structure of the deep fascia and its structural response to surgery. J Hand Surg (Brit), 2001;26:89-97.
- Roman M, Chaudhry H, Bukiet B, Stecco A, Findley TW. Mathematical analysis of the flow of hyaluronic acid around fascia during manual therapy motions. J Am Osteopath Assoc, 2013;113(8):600-10.
- Ercole B, Antonio S, Julie Ann D, Stecco C. How much time is required to modify a fascial fibrosis? J Bodyw Mov Ther, 2010;14(4):318-25.
Click here for previous articles by Warren Hammer, MS, DC, DABCO.





