When I write about the coccyx, I recognize that I am talking about a relatively small subset of patients. When I write for Dynamic Chiropractic, I am trying to reach 60,000 chiropractors.
Are you OK with being a pain doc? Are you OK with managing pain, rather than seeing yourself as the hero who cures pain? Your patient may start out with pain that is the center of their life. This is the patient who wears the "mask of pain"; the patient who has constant, severe pain. After treatment, whether it is two or 10 treatments, their pain levels may be down to a 2 or 3 out of 10, and may be present only 25-50 percent of the time. Can you be satisfied with this? Can you remind your patient to appreciate the half-full glass and to celebrate their ability to enjoy life?
First, a bit of back story. I am officially an elder now at age 66 and in practice for 35 years. I live in a town that is graying. Many of my patients range from 50-85 years old. I don't think I cure most of my patients. I think I help them manage their weak links, their chronic tendencies. And yes, that includes issues involving the coccyx.
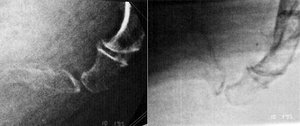
 Dislocation of the coccyx (left: standing; right: seated).
For the coccyx, we have a great screen, the dynamic lateral coccyx X-ray, which tells us if the problem is hypomobility or hypermobility. When the problem is hypomobility, our usual tools, manipulation and soft-tissue work, are likely to help. (I am a big rehab doc, but rehab is rarely the key for coccyx pain.) When the problem is hypermobility, the solution is less clear. When you are dealing with a hypermobile tailbone, you are solidly in the pain realm.
Dislocation of the coccyx (left: standing; right: seated).
For the coccyx, we have a great screen, the dynamic lateral coccyx X-ray, which tells us if the problem is hypomobility or hypermobility. When the problem is hypomobility, our usual tools, manipulation and soft-tissue work, are likely to help. (I am a big rehab doc, but rehab is rarely the key for coccyx pain.) When the problem is hypermobility, the solution is less clear. When you are dealing with a hypermobile tailbone, you are solidly in the pain realm.
If you are not going to cure the hypermobile coccyx, can you help these folks? The answer is a qualified yes or at least maybe. Let's explore how to identify the hypermobile coccyx and then manage or treat these patients.
When the Coccyx Moves Too Much: Dynamic Lateral Coccyx X-Rays
Can we actually measure and quantify joint motion? For the coccyx, we can at least measure whether there is excessive motion or a true dislocation. I am not normally a big X-ray or imaging guy. I rarely order films on my first visit with a patient, with an exception for coccyx pain that is either chronic or caused by trauma. Dynamic coccyx X-rays are both diagnostic and help determine prognosis.
Dynamic lateral coccyx X-rays were developed by Jean Yves Maigne, MD, of France. How is the imaging procedure done?1 Take a standing lateral coccyx X-ray first. Then have the patient sit on a hard surface. Have them sit for a couple of minutes, reproducing their typical pain, and then shoot a sitting lateral coccyx film. Compare the films, especially the angle of flexion at the sacro-coccygeal junction and between the segments of the coccyx. You are looking for excessive or aberrant motion. If you do not take in-house films, you will probably need to coach/train both the radiological tech and the reading radiologist on this protocol.
 Hypermobility of the coccyx (greater than 25 degree change of angle between standing and sitting). Images reprinted with permission from Jean Yves Maigne, MD.
The sitting X-ray is a form of provocation. It is likely to reproduce the patient's pain. Don't send the patient for X-rays immediately after you have mobilized their coccyx. This will undo any positive results they have gotten from the adjustment.
Hypermobility of the coccyx (greater than 25 degree change of angle between standing and sitting). Images reprinted with permission from Jean Yves Maigne, MD.
The sitting X-ray is a form of provocation. It is likely to reproduce the patient's pain. Don't send the patient for X-rays immediately after you have mobilized their coccyx. This will undo any positive results they have gotten from the adjustment.
There are two significant pathological findings you may miss without the sitting X-ray. One is dislocation: a coccyx that completely loses its normal relationship to the other coccygeal segments or the sacrum when sitting. In a dislocation, a segment of the coccyx has shifted or translated.
The second is hypermobility: a coccyx segment that has more than 25 degrees of motion (usually into flexion), comparing the standing film to the sitting film. Both of these findings represent excessive motion. The pictures below show these findings.
When you have either of these findings on the dynamic coccyx X-ray, you know there has been significant anatomical damage to the coccyx. In either of the above scenarios (dislocation or hypermobility), the ligaments are quite likely to be damaged and lax. I have talked a lot about functional hypermobility over the past few years. Here is a place where we can see and measure anatomical hypermobility. If the patient has excessive coccyx motion, it means something damaged those ligaments. This is a very small set of bones and ligaments which can be easily traumatized in a fall.
Over the years of using the internal coccyx exam and mobilization procedure, I have a pretty good idea of when the X-ray is going to show excessive motion. This is not always obvious, as this is an area where palpation is not easy or accurate. You have no visual cues and your database is likely to be extremely small. In some cases, it can feel as if the coccyx is just barely connected to the sacrum above, or the most distal segment feels as if it moves too easily. It's a very "wiggly" palpatory feel.
When the coccyx feels extremely stiff, both into flexion and into extension, it lends itself to manipulation. This is consistent with our basic motion palpation concept: mobilize the stuck segment. My previous articles on this topic are primarily about manipulation of the coccyx.2
 Yoga bow; hold for 15-60 seconds.
What conclusions can you draw after seeing the films? If they reveal a true anatomic pathology, either hypermobility or dislocation, you are less likely to get good results with manipulation. It does not mean you should not treat the patient; it does mean the prognosis is not as good. This is not an automatic "get the patient out of my office." First, relatively few medical specialists understand the coccyx. Second, if you take a pain perspective, you can help a lot of these folks, even if their ligaments have been damaged.
Yoga bow; hold for 15-60 seconds.
What conclusions can you draw after seeing the films? If they reveal a true anatomic pathology, either hypermobility or dislocation, you are less likely to get good results with manipulation. It does not mean you should not treat the patient; it does mean the prognosis is not as good. This is not an automatic "get the patient out of my office." First, relatively few medical specialists understand the coccyx. Second, if you take a pain perspective, you can help a lot of these folks, even if their ligaments have been damaged.
The Treatment Mindset
For the patient with a hypermobile coccyx, you need to have a different attitude. Your goal, as always, is to relieve the patient's pain and help them return to a more normal life. The critical message: You are trying to change the neural feedback loops. You are not putting a bone back in place. The context and the goal: change pain mechanisms; change the messages going from the brain to the tissue and vice versa. It is useful to look at all of your strategies from this neural perspective.
Your manipulation or other treatment is helping to break the vicious cycle. Pain reinforces pain. Nerves that fire together wire together. If you can change the feedback loop, it may change the long-term picture.
The mechanics are not the whole story. You know how imaging misleads us in relation to DJD and in relation to bulged or herniated discs. People with lousy-looking images often have no pain or respond well to conservative care, confounding the imaging-based prognosis.
So, what improves the prognosis? What tells you who is going to get well? The clearest indicator is based on a clinical audit protocol. Did you relieve the patient's pain with your treatment? Can they sit with more ease? Repalpate the painful area; does it feel less tender? If the answer to all or most of these questions is yes, the patient is likely to respond to your care.
Do this re-evaluation immediately after your treatment. On the second visit, ask the patient whether some of the pain relief lasted at least 24 hours.
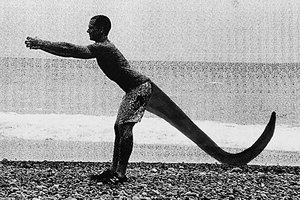 Dragon tail.
You can correct the hypermobile coccyx with mobilization, but it is harder to get it to stabilize. The old chiropractic phrase, "Does the adjustment hold?" comes into play here. If you are pulling an anterior coccyx backward and then the patient places the whole weight of their trunk on these small structures, it will often push the tailbone forward, back out of place.
Dragon tail.
You can correct the hypermobile coccyx with mobilization, but it is harder to get it to stabilize. The old chiropractic phrase, "Does the adjustment hold?" comes into play here. If you are pulling an anterior coccyx backward and then the patient places the whole weight of their trunk on these small structures, it will often push the tailbone forward, back out of place.
Nine Strategies for Treating the Hypermobile Coccyx
1. Sometimes, within the hypermobility, there are joints or fascial areas that lack mobility. When I am doing my internal procedures, I am not just pulling the tailbone backward. I am searching for what feels tender and stiff. I am attempting to differentiate which segment is tender and has abnormal tissue texture; which side is tender and stiff. I may release this through pressure, through positioning or through mobilization. The coccyx is at the end of the sacrum, so look at the sacrum and sacroiliac as well.
2. I have been strongly influenced by the osteopathic model. One of the differences in the osteopathic approach compared to the chiropractic approach is the emphasis on gentler and more indirect techniques. I think this is especially relevant for the type of coccyx pain we are discussing here, where excessive motion comes into play. Our goal is not just to unlock the stuck joint by direct pressure. Our goal is to help the tissues find ease.
For the practitioner, especially for the chiropractor trained in more direct forms of manipulation and soft tissue, this requires a different approach. I can't teach you these techniques in one paragraph of an article. But perhaps I can make you aware that gentler methods may be more effective in these types of cases. If all you have is a hammer, everything looks like a nail. I reference an exceptional (and long) article by Dr. Stephen Sandler.3
3. A third approach is soft-tissue oriented. This may mean you need to concentrate on soft-tissue work for the lateral musculature, fascia and ligaments when they are tender. The sacrotuberous ligaments, the gluteal origins and the coccygeus muscles are key here. These can be accessed externally, as well as from an internal approach. Laser treatment may fit in as well.
4. What about rehab? We recognize that any pain creates typical inhibitory patterns in the whole region of the pain. Helping the patient improve their core function may be useful, but it is rarely enough. If the coccyx is placed too far forward, extension and posterior-chain activation may be helpful. Anything you can do that gives the patient something they can do for their condition is empowering to them.
5. I have developed a couple of simple exercises that attempt to extend the coccyx region. These only work when the patient can tolerate end-range extension. They often relieve coccyx pain. The yoga bow is a form of extreme extension. The dragon tail4 is a variation on foundation training's "founder" maneuver,5 adding visualization of the coccyx being extended. If you are not familiar with foundation training, at minimum watch the linked video.
Again, I like to use a reality check. In the session in which I teach these exercises, I first palpate the tender coccyx, and then have the patient do the exercise. I then repalpate. If they have less pain on palpation, this exercise is likely to be useful to them.
6. I have just been introduced to taping and have not tried it yet. But it does make sense to me, from both a positioning and a proprioceptive sense, so I will include it. There is a simple taping protocol available.6 This is a stabilization form of taping; well-suited to the hypermobile joint. It uses McConnell-type taping to pull the coccyx posterior. The therapist who developed this mentioned she shows the patient and their partner how to do this themselves. I look forward to trialing it.
I suspect SPRT [specific proprioceptive response taping] might be equally effective, as it has a similar goal.
7. Pain-oriented injection procedures. We are talking about hypermobile areas. The pain generator is not primarily a lack of motion, but excessive or aberrant motion. Various kinds of injections can be helpful in breaking the cycle. If an injection gives lasting relief, the body / mind may forget about that pain. This may end up breaking the cycle permanently.
The older I get, the longer I am in practice, the less dogmatic I become. I cannot help everyone and I usually know after a few treatments whether I am helping someone or not. Don't reject injections because you don't do them. Don't reject this because it is not "natural medicine." Don't reject this because it is just treating the pain.
If your patient is not responding to your work, consider these approaches. Unfortunately, very few injection doctors, in my experience, have a clear protocol for what injections to use for the coccyx. I have linked to Dr. Patrick Foye's protocol.7
8. Prolotherapy injections. These are injections of glucose or other "proliferant" solutions. The goal is for the body to lay down repair tissue at the site of injection. Prolo could be curative when the patient has excess motion at the hypermobile coccyx. The downsides: The injections are painful, as they are pro-inflammatory; and insurance currently does not cover proliferant injections. (As much as I love my Graston technique, it does not seem applicable to the coccygeal ligaments, although I have used it on the more lateral sacrotuberous ligaments.)
9. If the patient gets no lasting relief from your work and/or injections, and they have evidence of anatomical damage, they may be a candidate for surgical removal of the anatomically damaged parts of the coccyx.
As always, start with the less invasive approaches and ramp up. You are going to help a significant percentage of these patients, even though their anatomy has been compromised.
References
- Maigne JY. "Management of Common Coccydinia," 2002, as reprinted on www.coccyx.org, with description of dynamic coccyx X-ray procedure.
- Heller M. "The Coccyx." Dynamic Chiropractic, Feb. 12, 2004; Heller M. "The Coccyx Revisited: External and Internal Exam Correction Procedures." Dynamic Chiropractic, Feb. 26, 2010,
- Sandler S. "The Coccyx for Osteopaths," 2014, published on the Waltham Forest Osteopathy Group website; a long and good article.
- Original picture courtesy of foundation training; dragon tail imagery concept thanks to Kathleen Pagnini (http://kathleenpagnini.com).
- Demonstration of "the Founder" by Eric Goodman, creator of foundation training.
- "Taping Technique to Treat Coccyx Pain." Coccyx taping technique with good pics available at www.coccyx.org.
- "3 Different Injections for Tailbone Pain." Protocol for coccyx injections available on www.tailbonedoctor.com.
Click here for more information about Marc Heller, DC.





