Accessory ossicles in the foot are abundant, making it difficult to assess whether or not there is a fracture.
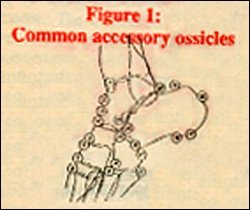
- os talotibiale
- os supratalare
- an avulsion, not an accessory bone
- os supranaviculare
- os infranaviculare
- os intercuneiforme
- os cuneometatarsale II dorsale (also os cuneometatarsale dorsale fibulare)
- os intermetatarsale
- os unci? Coalescing with the fourth metatarsal bone?
- accessory skeletal element distal to the cuboid (wandering os unci?)
- secondary cuboid (cuboides secundarium)
- calcaneus secundarius
- os tibiale externum
- trigonum
- os accessorium supracalcaneum
- posterior calcaneal spur, not an accessory bone
- os subcalcis
- inferior calcaneal spur, not an assessory bone
- bursitis, not an accessory bone
- peroneal bone (os peroneum)
- os vesalianum
Most of the time a simple evaluation of the opposite foot will allow one to differentiate most fractures from an accessory ossicle.
One of the most commonly missed fractures that can be mistaken as an accessory ossicle is an avulsion fracture at the base of the fifth metatarsal. Avulsion of the styloid process of the fifth metatarsal are caused by an inversion injury to the ankle, stressing the peroneus brevis tendon which causes an avulsion at the insertion of this tendon.
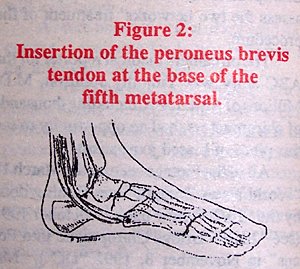
Usually the patient will describe a history of stepping off a curb or falling down the stairs. Clinically, this fracture initially appears to be an injury to the ankle, due to the marked swelling which occurs over the lateral aspect of the ankle. If only ankle films are taken, this fracture will be missed.
This fracture can also be confused with the os peroneum. Radiographically these two entities can be differentiated by the direction of the fracture line. The fracture line is usually oriented transversely in relationship to the base of the matatarsal. In contrast, when an os peroneum is present, the line of separation is usually obliquely longitudinal in relationship to the base of the metatarsal.
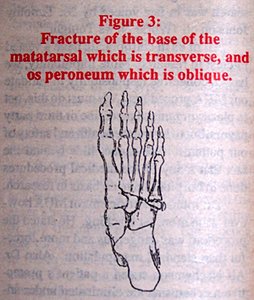
If the fracture is non-displaced, a compression bandage can be used along with restricting weight-bearing until the edema has resolved. If the fracture is displaced, the ankle and foot should be immobilized in the neutral position. Referral to an orthopedist or podiatrist would be recommended for proper management unless the chiropractor is proficient in casting techniques and fracture management. Ice and pulsed ultrasound also can be very helpful in reducing the edema. It should be noted that if the fracture remains open after nine months and is still symptomatic, surgical intervention may be necessary.
Deborah Pate, D.C., DACBR
San Diego, California
Editor's Note:
Dr. Pate's book, Case Studies in Chiropractic Radiology is now available through MPI's Preferred Reading and Viewing list. Please see pages xx, Part #T123 for further information on how to order your copy.
Click here for more information about Deborah Pate, DC, DACBR.





