Calcification of the laryngeal cartilages often is confused with possible calcification in the thyroid gland. We don't want to miss calcification involving a tumor in the thyroid, but we don't want to alarm patients unnecessarily and request expensive (financially and emotionally) tests and procedures.
The thyroid is the most common endocrine organ to undergo malignant degeneration; however, thyroid carcinoma accounts for only 1 percent of diagnosed neoplasms in the U.S. annually. Thyroid cancer is rare; the annual detection rate of clinically significant thyroid cancer in the general population is only 0.004 percent. Only 5-10 percent of thyroid cancers are clinically palpable. Keeping in mind that the thyroid gland sits below the thyroid cartilage beginning at the C5 level, and can extend as low at T1, it should be fairly easy to differentiate pathologic calcification from physiologic calcification.
In general, when the thyroid enlarges it will extend inferiorly. In all my years of reviewing films, I have yet to see a thyroid tumor that had calcifications visible on a cervical X-ray series. This does not mean the possibility should not be considered. If there is calcification, most of the time it is very discrete and difficult to visualize on X-ray unless the tumor is large. The calcifications are better seen on ultrasound studies or a CT scan.
When the tumor is large enough to be palpable, it will often cause a deviation in the trachea. Knowing the ossification patterns of the laryngeal cartilage and other possible physiologic calcifications in the anterior aspect of the neck will help avoid unnecessary procedures.
Primer on Laryngeal Cartilages
There are three unpaired (thyroid, epiglottis and cricoid) and three paired (arytenoid, cuneiform and corniculate) laryngeal cartilages. (Fig. 1) Thyroid cartilage consists of two laminae that meet at midline anteriorly. Posteriorly, they curve superiorly, forming superior cornua; and inferiorly forming the inferior cornua. Inferior cornua articulate with cricoid cartilage inferiorly.
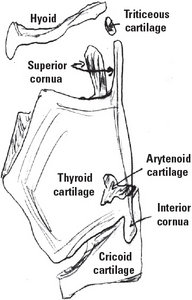 Fig. 1: Laryngeal cartilages.
Cricoid is a signet ring-shaped cartilage that lies below the level of thyroid cartilage. It consists of posterior lamina and a narrow anterior arch. Arytenoid cartilages are small, paired cartilages superior to cricoid cartilage. The base of the arytenoids rest on cricoid cartilage. Triticeous cartilages are small, elastic cartilages that lie at the thyrohyoid membrane.
Fig. 1: Laryngeal cartilages.
Cricoid is a signet ring-shaped cartilage that lies below the level of thyroid cartilage. It consists of posterior lamina and a narrow anterior arch. Arytenoid cartilages are small, paired cartilages superior to cricoid cartilage. The base of the arytenoids rest on cricoid cartilage. Triticeous cartilages are small, elastic cartilages that lie at the thyrohyoid membrane.
Thyroid, cricoid and most of the arytenoid cartilages are hyaline cartilages that undergo enchondral ossification as people age. Apices of arytenoids, epiglottis, corniculate and cuneiform cartilages are elastic cartilages that will not calcify. Triticeous cartilages are variable small, elastic cartilages that calcify.
Normal Calcification / Ossification Patterns
Thyroid cartilage calcification / ossification starts by 20-25 years of age at the postero-inferior part of the lamina and inferior cornua. It then progresses upward and anteriorly. So, it is unusual to see isolated superior lamina or superior cornua ossification. Eventually, male thyroid cartilage completely ossifies, whereas in females the anterior aspect is left unossified. The thyroid cartilage calcification/ossification is used in forensics to determine the age of a person when other anatomical structures are missing.
Cricoid and arytenoid cartilages calcify in the third decade, but somewhat later than thyroid cartilage. The superior margin and lamina of the cricoid ossify earlier than other parts. Ossification of the cricoid can be identified even in the presence of thyroid cartilage ossification. Arytenoid calcification starts from the base of arytenoids sitting on the upper aspect of the cricoid lamina. When completely calcified, it has an L-shaped appearance.
 Fig. 2: Laryngeal cartilage calcifications: a) Triticeous, b) Superior cornua, c) Thyroid and d) Cricoid.
Triticeous cartilages are variable. When present and calcified, they can be seen along the line between superior cornua of the thyroid and the posterior part of the greater cornua of the hyoid.
Fig. 2: Laryngeal cartilage calcifications: a) Triticeous, b) Superior cornua, c) Thyroid and d) Cricoid.
Triticeous cartilages are variable. When present and calcified, they can be seen along the line between superior cornua of the thyroid and the posterior part of the greater cornua of the hyoid.
The pattern and rate of calcification / ossification can vary among individuals and are unpredictable. They can appear in unexpected and disordered patterns as well. Calcification becomes denser in appearance as age advances. Knowledge of the anatomical location and pattern of cartilage calcification is helpful when determining whether there is a foreign body or calcification in the thyroid gland. The thyroid cartilage is seen at the level C3-C5 and C6 for cricoid. (Fig. 2) The thyroid gland sits at the C5 level and extends inferiorly to the T1 level in some people.
Differentiating Other Calcifications in the Neck
Other calcifications in the neck such as the styloid process, the stylohyoid ligament and the hyoid bone are easily identified and should never be confused with calcifications in the thyroid gland, since they are not even near these structures anatomically. Vertebral osteophytes and anterior longitudinal ligament ossification generally are also easily identified due to their close relationship to the vertebrae and, as in ossification of the anterior longitudinal ligament, as a continuous, linear band of ossification close to anterior vertebral body margins.
Tracheal cartilage can also calcify with advancing age, but should not be difficult to identify due to the ring-like appearance. Lymph node and vascular calcification should be recognizable once correlated with their location on the AP view.
Click here for more information about Deborah Pate, DC, DACBR.





