Editor's Note: Part 1 this article appeared in the December 2022 issue.
A Simple Screening Solution
There is a tradeoff between DEXA and CT, but now it can be avoided. When CTs are obtained for other reasons, the data can be used "opportunistically" to screen for osteoporosis. Part of the increased cost of traditional QCT is the requirement for specialized calibration phantom and analysis software.
An interesting statistic reported at the RSNA in 2019 was that fewer than 6 percent of older women (age > 65 years) who have undergone CT of the chest or abdomen have undergone a DEXA examination.4 This is an important realization; more postmenopausal women have had a CT scan than have had a DEXA scan.
Are we missing something? The CT scan has become an extremely common imaging modality, but what is not common is "opportunistic CT." That is to say, we are not taking advantage of the secondary analysis of existing CTs to obtain quantitative body composition data without additional testing.5-6
More importantly, concerns about the higher radiation exposure of CT compared to DEXA become moot when BMD measurements are analyzed on CT exams that are already being performed for other indications. And opportunistic CT evaluation becomes particularly important for patients who would otherwise not undergo DEXA testing.
Nowadays, opportunistic CT is a rapid and reproducible method of screening patients for osteoporosis, and may even show significant bone loss before it can be detected with DEXA. CT technology has advanced so that the Hounsfield units (HU) values can be used in screening for osteoporosis in patients during routine CT abdomen, pelvis and lumbar spine scans performed for other diagnostic reasons.
Hounsfield Unit (HU) values (Table) measured from the diagnostic CT images can be correlated with the BMD and the T-score measured by DEXA, thus obviating the need to do another test like DEXA for BMD assessment.7
|
|
||
CT HU VALUES FOR TISSUES OF THE BODY |
||
|
|
||
Predefined Threshold Value |
Minimum |
Maximum |
|
|
||
| Bone (CT) | 226 | 3071 |
|
|
||
| Soft Tissue (CT) | -700 | 225 |
|
|
||
| Enamel (CT, Adult) | 1153 | 2850 |
|
|
||
| Enamel (CT, Child) | 2042 | 3071 |
|
|
||
| Compact Bone (CT, Adult) | 662 | 1988 |
|
|
||
| Compact Bone (CT, Child) | 586 | 2198 |
|
|
||
| Spongial Bone (CT, Adult) | 148 | 661 |
|
|
||
| Spongial Bone (CT, Child) | 156 | 585 |
|
|
||
| Muscle Tissue (CT, Adult) | -5 | 135 |
|
|
||
| Muscle Tissue (CT, Child) | -25 | 139 |
|
|
||
| Fat Tissue (CT, Adult) | -205 | -51 |
|
|
||
| Fat Tissue (CT, Child) | -212 | -72 |
|
|
||
| Skin Tissue (CT, Adult) | -718 | -177 |
|
|
||
| Skin Tissue (CT, Child) | -766 | -202 |
|
|
||
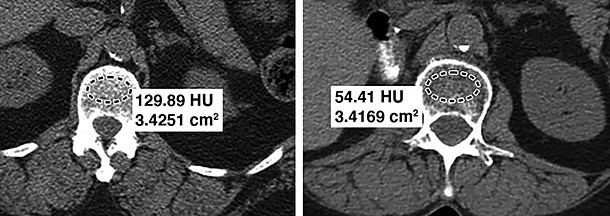
Measurements for osteoporosis in the spine are generally taken at the specific thresholds at the L1 level. If the vertebral body has an attenuation of 90 HU or less, it is considered to be osteoporosis; conversely, attenuation of more than 160 HU essentially rules out osteoporosis.7-8 Fig. 1 demonstrates two different patients: one with normal bone density and the other with osteoporosis.
Another Diagnostic Benefit
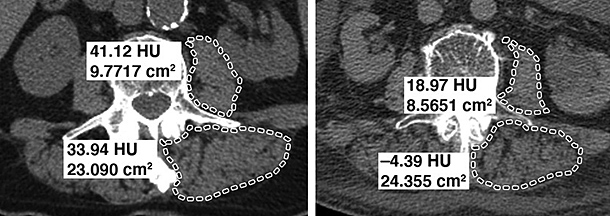
Another very common and overlooked disorder that is age related and often associated with osteoporosis is sarcopenia, which also can be identified on CT as decreased muscle mass and low attenuation. The finding on CT is that skeletal muscle has fat infiltration (known as myosteatosis).
Several studies show that sarcopenia is an independent predictive factor of high fracture risk besides BMD and other clinical conditions; and that an association exists among sarcopenia, risk of falls and osteoporotic fractures.9-10 It is clear that the two conditions, sarcopenia and osteoporosis, are closely correlated, and that their combination leads to exacerbation of negative health effects and to frailty syndrome development.11 The point is that both bone density and muscle density can be accessed on CT "opportunistically."
CT-derived thresholds for diagnosing low muscle mass and attenuation have been established; the current diagnostic threshold is 30 HU for both the psoas and paraspinal muscles, so any measurement lower than 30 HU is indicative of myosteatosis. (Fig. 2)
Measurements for osteoporosis in the spine are generally taken at the specific thresholds at the L1 level. If the vertebral body has an attenuation of 90 HU or less, it is considered to be osteoporosis; conversely, attenuation of more than 160 HU essentially rules out osteoporosis.7-8 Fig. 1 demonstrates two different patients: one with normal bone density and the other with osteoporosis.
Best-practice standards for the diagnosis, prevention and treatment of sarcopenia are developing, but we as chiropractors have an opportunity to treat patients who otherwise will fall through the gaps in our health care system.
We now can add further value to routine imaging with the use of CT biomarkers that assess bone and muscle health – without additional examination time or additional radiation, helping patients mitigate or avoid the immense negative consequences associated with osteoporosis and sarcopenia.
References (Pt. 1 & Pt. 2)
- Facts About Osteoporosis: www.health.ny.gov/publications/2047/.
- De Luca K, Hogg-Johnson S, Funabashi M, et al. The profile of older adults seeking chiropractic care: a secondary analysis. BMC Geriatr, 2021 Apr 23;21(1):271.
- Kulkarni AG, Thonangi Y, Pathan S, et al. Should Q-CT be the gold standard for detecting spinal osteoporosis? Spine, 2022 Mar 15;47(6):E258-E264.
- Barton DW, Behrend CJ, Carmouche JJ. Rates of osteoporosis screening and treatment following vertebral fracture. Spine J, 2019 Mar;19(3):411-417.
- Lenchik L, Weaver AA, Ward RJ, et al. Opportunistic screening for osteoporosis using computed tomography: state of the art and argument for paradigm shift. Curr Rheumatol Rep, 2018 Oct 13;20(12):74.
- Boutin RD, Lenchik L. Value-added opportunistic CT: insights into osteoporosis and sarcopenia. Am J Roentgenol, 2020 Sep;215(3):582-594.
- Zhang D, Wu Y, Luo S, et al. Cha racteristics of lumbar bone density in middle-aged and elderly subjects: a correlation study between T-scores determined by the DEXA scan and Hounsfield units from CT. J Healthc Eng, 2021 Dec 16;2021:5443457.
- Alawi M, Begum A, Harraz M, et al. Dual-energy X-ray absorptiometry (DEXA) scan versus computed tomography for bone density assessment. Cureus, 2021 Feb 10;13(2):e13261.
- Greco EA, Pietschmann P, Migliaccio S. Osteoporosis and sarcopenia increase frailty syndrome in the elderly. Front Endocrinol (Lausanne), 2019 Apr 24;10:255.
- Yu R, Leung J, Woo J. Incremental predictive value of sarcopenia for incident fracture in an elderly Chinese cohort: results from the Osteoporotic Fractures in Men (MrOs) Study. J Am Med Dir Assoc, 2014 Aug;15(8):551-8.
- Testa G, Vescio A, Zuccalà D, et al. Diagnosis, treatment and prevention of sarcopenia in hip fractured patients: where we are and where we are going: a systematic review. J Clin Med, 2020 Sep 17;9(9):2997.
Click here for more information about Deborah Pate, DC, DACBR.





