Those of my readers who know me from my seminars know that I occasionally buck the system. No, I'm not much of an iconoclast, but sometimes that trait has gotten me into trouble. Like the bumper sticker of the '70s, I say question authority.
Range of motion (ROM) is an example of something that has become almost a universally accepted yardstick of spinal health or function. While medical associations and societies struggled to arrive at normal values for spinal ROMs (usually through a consensus process) and then, having done that, set out to devise methods of correlating limitations of these normal ranges with patient impairment, few ever questioned whether limitations of motion do actually correlate with disability or impairment. In fact, this yardstick appears to be elastic and poorly calibrated. Most physicians subscribe to the figures put out by the AMA (guidelines) or the American Academy of Orthopaedic Surgeons when it comes to spinal ranges of motion. Yet, despite the fact that it has been known for many years that some variance in ROM exists between the genders and that ROM gradually diminishes with time,1 these associations have apparently not considered these variances significant. Moreover, they have not revealed the source of their data. More recently Youdas et al.,2 have looked anew at this subject of age and gender-based ROM variance and have subjected their results to statistical analysis. They've also published regression equations that can be used to calculate the patient's normal ROM based on gender and age.
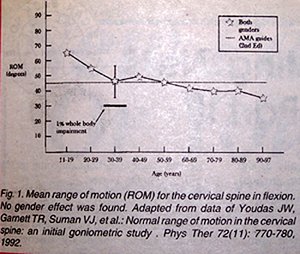
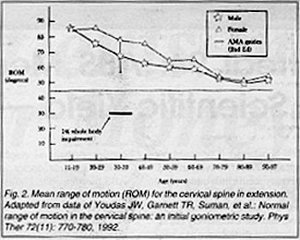
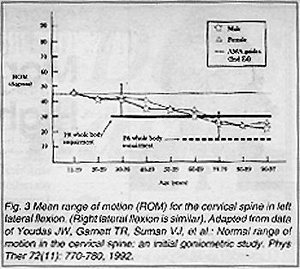
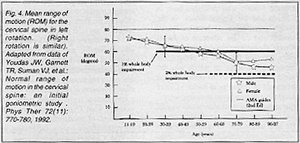
I've taken some of their raw data and graphed it to demonstrate some of this variation (Figures 1-4). Notice that the dashed line represents the AMA guidelines for normal ROM. The values in the figures represent means only. When I calculated the lowest values in the normal distribution (i.e., minus two standard deviations, vertical bars), many of these values fell within ranges that would be given 1-2 percent whole body impairments by strict AMA guidelines.
If these were the only problems with ROM, we could easily enough modify our paradigm. But how do we account for variations within the same patient? How do we know that measured limitations are not merely the result of a transient inflammatory effect or muscle spasm. Medicolegal evaluators usually rely on a single recording of ROM. An erroneous measurement could have a profound effect on a disability award. And ROM can be affected by mobilization and manipulation.3 Moreover, there seems to be no universally accepted method of measuring ROM, with some authors recording active ROM and others recording passive ROM. Wong and Nansel have described the difficulty of interpreting such recordings.4 And then there is the issue of instrumentation. In one study, the universal goniometer was found to be as accurate as more sophisticated instruments measuring cervical ROM.5 In a more recent study, Chiarello and Savidge reported no significant differences in inter-rater reliability comparing digital goniometers and fluid goniometers.6
I find it curious that the AMA now suggests clinicians use the inclinometer, apparently to arrive at a more precise measurement, despite the fact that their normative data, which fails to consider either gender or age, is anything but precise.
Several studies have attempted to correlate limitations of motion (either gross or intersegmental) with pain or impairment and have failed to make that connection.7,8,9 Perhaps most instructive is a report from Lowery et al.10 These authors measured the cervical and lumbar ROMs of 81 healthy subjects using the double inclinometer method. Based on AMA criteria, virtually all of these normal subjects were found to have some degree of impairment ranging from a low of two percent to a high or 38.5 percent, with a mean of 10.8 percent. Not surprisingly, the level of impairment increased with age, again calling attention to the shortcomings of the AMA's current set of normal values.
Until we can address some of these issues more pragmatically, we must be careful not to allow limitations of motion to adumbrate the clinically relevant factors that truly impair our patients. Embracing motion limitations as the sole objective evidence of impairment may just be an example of a wrong question inviting an irrelevant answer.
References
- Ferlic D. The range of motion of the "normal" cervical spine. Johns Hopkins Hosp Bull, 110:59-65, 1962.
- Youdas JW, Garrett TR, Suman VJ, et al. Normal range of motion of the cervical spine: an initial goniometric study. Phys Therapy, 72(11):770-780, 1992.
- Cassidy JD, Lopes AA, Yonghing K. The immediate effect of manipulation vs. mobilization on pain and range of motion in the cervical spine -- a randomized trial. JMPT, 15(9):570-575, 1992.
- Wong A, Nansel DD. Comparisons between active vs. passive end-range assessments in subjects exhibiting cervical range of motion asymmetries. JMPT, 15(3):159-163, 1992.
- Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion comparison of three methods. Phys Therapy, 71(2):98-104, 1991.
- Chiarello CM, Savidge R. Inter-rater reliability of the Cybex EDI-320 and fluid goniometer in normals and patients with low back pain. Arch Phys Med Rehab, 74:32-37, 1993.
- Hamalainen O, Vanharanta H, Bloigu R: Determinants of +Gz- related neck pain -- a preliminary survey. Aviat Space Environ Med, 64(7):651-652, 1993.
- Tsai L, Wredmark T. Spinal posture, sagittal mobility, and subjective rating of back problems in former female elite gymnasts. Spine, 18(7):872-875, 1993.
- Haas M, Nyiendo J. Lumbar motion trends and correlation with low back pain. A roentgenological evaluation of quantitative segmental motion in lateral bending. JMPT, 15(4):224-234, 1992.
- Lowery WD, Horn TJ, Boden SD, Wiesel SW. Impairment evaluation based on spinal range of motion in normal subjects. J Spinal Disord, 5(4):398-402, 1992.
Arthur Croft, DC, MS, FACO
San Diego, CA
Click here for previous articles by Arthur Croft, DC, MS, MPH, FACO.





