What are the indications for motor control exercises? Is it rarely if ever indicated? Is it universally indicated like many chiropractors believe adjustments are? When to perform a certain procedure is just as important as how to perform it.
A number of recent papers have demonstrated that spinal instability or poor motor control can be identified and correlated with musculoskeletal pain. Thus, indications for specific adjustments or exercises which can improve motor control now exist.
Relationship between Instability and Pain
A fascinating paper published last year in the journal Pain presented objective evidence that low back pain has a predictable effect on gait.1 Specifically they found:
- characteristic increases in muscle activity occur during gait in LBP patients; increased EMG activity in ipsilateral longissimus muscle during swing phase;
- decreased agonist muscle force;
- increased antagonist muscle output.
- difficulty with righting and postural reactions;
- standing with their center of force (COF) posterior, which increases their body sway and reduces motor control at the ankle;
- difficulty shifting their COF to the weight-bearing limb when standing on one leg.
McGill in the soon to be published ACSM Resource Manual states, "Generally, the better exercise programs are designed to train the motor control system to activate the spine stabilizers, then to progress with endurance training, and then finally to enhance strength and flexibility."4 Stabilization exercises have been shown to improve motor control at the lumbopelvic joints.5 These exercises involved training kinaesthetic awareness of how to perform a posterior pelvic tilt without increasing lumbar lordosis. Balance exercises have been shown to improve muscle activation in the pelvic area and lower extremity.6,7 Balogun found that a wobble board training program resulted in training effects "which were not limited to one muscle group, but affected muscles that span the hip, knee and ankle joints."7
How, When and Why to Train Key Stabilizers:12,13
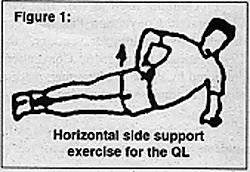
1) Quadratus Lumborum (QL)
Why: According to McGill the QL is the most active lumbar muscle during activities of daily living.8 It is a primary stabilizer of the spine. Although the QL is a muscle which tends to tightness (according to Janda), it is often both tight and weak.When
- Any time there is inhibition of the gluteus medius confirmed by the gait analysis, one leg standing test, or the side lying hip abduction test.
- Any time there is confirmation of a myofascial involvement of the QL by the presence of a trigger point (Travell, Simons criteria).
How
- Begin by inhibiting overactivity of the QL.
PIR of the QL.
- Then facilitate the gluteus medius.
PIR to TFL, adductors, piriformis and/or QL;
Rocker board;
1 leg bridges.
- Train the QL with the horizontal side support exercise. Train for endurance - gently with long isometric holds.
2) Multifidus
Why
- This is a primary intersegmental stabilizer of the spine. * It has a short reaction time due to its location near the center of rotation of the vertebrae. * It is the primary muscle active during static back extensor endurance testing (i.e., Sorensen's test), where poor endurance has been found to be able to predict 1st time onset of LBP in healthy individuals and recurrence rates in those recovering from LBP.9-11
- Increased lordosis is a sign of a poor hip extension movement pattern. This is due to overactivity of the iliocostalis lumborum or longissimus thoracis and inhibition of the multifidus. * Type 2 fiber atrophy has been found in chronic LBP and disc patients. * Moth eaten changes have been confirmed in type 1 fibers * Atrophy has been found in acute LBP patients and was improved with stabilization training.
When
- any time there is a positive Sorensen test, especially if the lumbar spine hyperlordosis or there is shaking during the test; * any time there is hyperlordosis during the hip extension test or during gait.
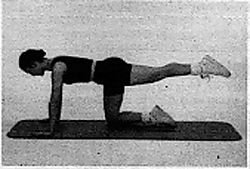
How
- Begin by inhibiting overactivity of the multifidus. CMT to dysfunctional lumbar segments; PIR of the multifidus (see Lewit). * Then train kinaesthetic awareness (KA) of abdominal hollowing. If KA training is difficult utilize propriosensory training. * If necessary, relax or stretch the iliopsoas or superficial erector spinae to reduce hyperlordosis during hip hyperextension. * Perform quadruped stabilization exercises, avoiding hyperlordosis (see Figure 2). If leg extensions cannot be performed without hyperlordosis, "peel-back" to: -- bridges; -- prone partial hip extension over a pillow w/a posterior pelvic tilt.
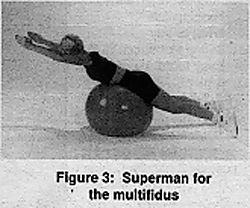
- Train the superman exercise (see Figure 3) and consider the roman chair as an option (train for endurance).
Figure 3: Superman for the multifidus.
Conclusion
These exercises and their indications are taught in the Chiropractic Rehabilitation Diplomate program. The skills necessary to effectively integrate these procedures into your practice are taught in small group workshops, facilitated by teaching assistants in the LACC program. Many of the articles listed here are available from a new rehabilitation literature file available from LACC's library. Please contact the library at (310) 947-8755.References
- Arendt-Nielsen et al. Pain 64:231-240, 1995.
- Byl N. Spine Vol 16:3, 1991
- Babyar SR. Phys Ther 1996;76:226-238..
- McGill S. ACSM Resource Manual 3rD ED
- Elia DS, Bohannon RW, et al. Dynamic pelvic stabilization during hip flexion. JOSPT, 1996:(21) 30-36.
- Bullock -Saxton JE, Janda V, Bullock MI. Reflex activation of gluteal muscles in walking. Spine 18:6;704-708, 1993.
- Balogun J, Adesinasi C, Marzouk D. The effects of a wobble board exercise training program on static balance performance and strength of lower extremity muscles. Physio Canada 1992;(44) 23-30.
- McGill S, et al. Quantitative intramuscular myoelectric activity of the quadratus lumborum during a wide variety of tasks. Clin Biomechanics 1996;11(3);170-2.
- Ng J, Richardson C. Reliability of electromyographic power spectral analysis of back muscle endurance in healthy subjects. Arch Phys Med Rehabil 1996;77:259-264.
- Biering-Sorensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine 1984;9: 106-119.
- Luoto S, Heliovaara M, Hurri H, Alaranta H. Static back endurance and the risk of low-back pain. Clin Biomech 10:6;323-324, 1995.
- Hyman J, Liebenson C. Spinal stabilization exercise program. In Liebenson C (ed) Spinal Rehabilitation: A Manual of Active Care Procedures. Williams and Wilkins, Baltimore 1996.
- Oslance J, Liebenson C. The prorio-system. Exerball products (800) 393-7255 or (619) 673-1733, San Diego, 1996.
Click here for previous articles by Craig Liebenson, DC.