 Fig. 1: AP view of the knee.
There are a few common normal variants that are viewed on a knee series that can appear as pathology. A limited series of the knee consists of AP, lateral and sunrise views. The AP view of the knee (Fig. 1) can be performed with the patient either supine or weight-bearing. It can be performed with or without a grid technique. The central ray is angled 5 degrees cephalad and enters at the inferior margin of the patella. The main areas to evaluate are the joint space between the femur and tibia, the integrity of the bones and alignment. The adjacent soft tissues should also be evaluated. There are two common findings that are normal variants: an accentuated groove for the popliteal tendon in the lateral condyle and bipartite patella.
Fig. 1: AP view of the knee.
There are a few common normal variants that are viewed on a knee series that can appear as pathology. A limited series of the knee consists of AP, lateral and sunrise views. The AP view of the knee (Fig. 1) can be performed with the patient either supine or weight-bearing. It can be performed with or without a grid technique. The central ray is angled 5 degrees cephalad and enters at the inferior margin of the patella. The main areas to evaluate are the joint space between the femur and tibia, the integrity of the bones and alignment. The adjacent soft tissues should also be evaluated. There are two common findings that are normal variants: an accentuated groove for the popliteal tendon in the lateral condyle and bipartite patella. AP View
 Fig. 2: Popliteal groove.
Fig. 2: Popliteal groove.
|
 Fig. 3: Popliteus muscle.
Fig. 3: Popliteus muscle.
|
 Fig. 4: Bipartite patella.
Fig. 4: Bipartite patella.
|
 Fig. 5: Normal and bipartite patella.
The AP tunnel view demonstrates an accentuated groove (Fig. 2, white arrow) for the patellar tendon, which is a normal finding and should not be confused with erosion. The popliteus muscle origin is on the anterior portion of the popliteal groove on the lateral femoral condyle; a lesser origin is from the head of the fibula, and there is an additional origin from the lateral meniscus in a small percent of the population (Fig. 3). It courses under the lateral collateral ligament, descends into the popliteus hiatus, then passes under the arcuate ligament and becomes extra-articular before finally joining its muscle belly. It's insertion is fan-like on the posterior surface of the tibia above the popliteal line.
Fig. 5: Normal and bipartite patella.
The AP tunnel view demonstrates an accentuated groove (Fig. 2, white arrow) for the patellar tendon, which is a normal finding and should not be confused with erosion. The popliteus muscle origin is on the anterior portion of the popliteal groove on the lateral femoral condyle; a lesser origin is from the head of the fibula, and there is an additional origin from the lateral meniscus in a small percent of the population (Fig. 3). It courses under the lateral collateral ligament, descends into the popliteus hiatus, then passes under the arcuate ligament and becomes extra-articular before finally joining its muscle belly. It's insertion is fan-like on the posterior surface of the tibia above the popliteal line.
 Fig. 6: Lateral view of the knee.
The bipartite patella is a normal variant and can be confused with a fracture (Fig. 4). There are three classifications: type I, inferior pole of the patella; type II, lateral margin; and type III superolateral type, which is the most common (Fig. 5). Differential diagnosis includes a stress fracture. Look for a vertical fracture line. Sinding-Larsen-Johansson disease may resemble a type I bipartite patella, patellar sleeve fracture and osteochondral fracture. History of trauma, hemarthrosis of the knee, point tenderness over defect, distinct outline of fracture on films, unilateral defect or MRI of the knee will demonstrate recent fracture or injury. These will help distinguish these disorders from bipartite patella.
Fig. 6: Lateral view of the knee.
The bipartite patella is a normal variant and can be confused with a fracture (Fig. 4). There are three classifications: type I, inferior pole of the patella; type II, lateral margin; and type III superolateral type, which is the most common (Fig. 5). Differential diagnosis includes a stress fracture. Look for a vertical fracture line. Sinding-Larsen-Johansson disease may resemble a type I bipartite patella, patellar sleeve fracture and osteochondral fracture. History of trauma, hemarthrosis of the knee, point tenderness over defect, distinct outline of fracture on films, unilateral defect or MRI of the knee will demonstrate recent fracture or injury. These will help distinguish these disorders from bipartite patella.
Lateral View
The lateral view of the knee (Fig. 6) can be performed with the patient lying on their side or weight-bearing. It can be performed with or without a grid technique. Most often the view is performed with the patient lying on their side with the lateral aspect of the knee closest to the film. The knee is flexed about 45 degrees and the central ray at the joint space angles 12 degrees cephalad. If performed standing, the patient can place the symptomatic side closest to the bucky and place their foot up on a low stool.
 Fig. 7: Osgood-Schlatter disease.
Fig. 7: Osgood-Schlatter disease.
|
 Fig. 8: Normal apophysis tibia.
Fig. 8: Normal apophysis tibia.
|
The cephalad angle may not work if the patient is standing, depending on their height and the range of the X-ray tube. The main areas to evaluate are the joint space between the femur and tibia, and the joint space between the femur and patella. Of course, the integrity of the bones and alignment should be evaluated.
There are three common variants that can seen on this view. The fabella, a common sesamoid bone in the lateral head of the gastrocnemius muscle, occurring in 10 to 30 percent of individuals, is seen on this lateral view of the knee (Fig. 6). The second common variant is the tibial tuberosity, which can appear like an avulsion fracture of the tibial tuberosity. It is sometimes difficult to determine if there is an avulsion fracture or just an unfused apophysis. The epiphyseal region of the tibial head forms a beak-shaped process that extends downward anteriorly over the tibia at its distal end. There is an isolated ossification center which forms the tuberosity.
 Fig. 9: Pseudoperiostitis.
Fig. 9: Pseudoperiostitis.
|
 Fig. 10: Pseudoperiostitis.
Fig. 10: Pseudoperiostitis.
|
This appears at about the 7th or 15th year and needs to be differentiated from Osgood-Schlatter disease, which is mainly a clinical diagnosis rather than a radiographic one. These lateral views of two different patients (Figs. 7 and 8) appear similar. Without clinical finding, both could be called normal. The patient must have the associated pain and tenderness at the tibial tuberosity; radiographic findings are secondary.
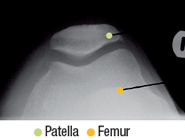 Fig.11: Sunrise view of the patella.
The third common finding that can be confused with pathology is an irregularity in the posterior margin of the distal femur, which is termed pseudoperiostitis (Figs. 9 and 10). This finding can also be observed at the attachments of the interosseous membrane on the tibia and fibula. This finding is mainly seen in younger individuals and needs to be differentiated from the periosteal bone reaction associated with aggressive neoplasms involving bone.
Fig.11: Sunrise view of the patella.
The third common finding that can be confused with pathology is an irregularity in the posterior margin of the distal femur, which is termed pseudoperiostitis (Figs. 9 and 10). This finding can also be observed at the attachments of the interosseous membrane on the tibia and fibula. This finding is mainly seen in younger individuals and needs to be differentiated from the periosteal bone reaction associated with aggressive neoplasms involving bone.
Sunrise View
The third view performed of the knee in a limited knee series is the sunrise view (Fig 11), performed with the patient prone with the knee in extreme flexion, with or without a grid technique. The central ray is at about the superior-most anterior surface of the patella. If the patient can not flex sufficiently, a cephalad tube tilt can be used. This view is performed mainly to evaluate the articulation of the patellofemoral joint. There is a variation in the shape of the patella but the medial and lateral joint spaces should be similar, and the apex of the patella should align with the deepest part of the intercondylar sulcus.
For a more in-depth review of normal variants, review Theodore Keats' Atlas of Normal Roentgen Variants That May Simulate Disease.
Click here for more information about Deborah Pate, DC, DACBR.





